Causes and pathogenesis of alcohol dependence. Etiology of alcoholism. Causes and mechanisms of development of alcoholism. Chronic alcohol use
Causal factor of alcoholism is ethyl alcohol, ethanol, whose action determines drug addiction. Personal, social (microsocial) and physiological factors contribute to the development of the disease.
Our knowledge physiological factors are still at the level of speculation. This is explained by the fact that various biochemical and physiological changes found in alcoholism cannot be completely extrapolated to the premorbid period. The pathology found in alcoholism can rightfully be considered as a reflection of pathogenesis, but not as a manifestation of those physiological characteristics that determined the development of alcoholism.
However undoubtedly that physiological prerequisites for the development of alcoholism exist. Proof of this is the fact that alcoholism develops at different times in different people with the same degree of intoxication. There are known cases of systematic consumption of alcoholic beverages, in which it remains possible to regulate further alcoholism. And, conversely, there are often cases of very rapid formation of drug addiction to alcohol within a few months.
Fast formation alcoholism possible when the external conditions that determine the physiological background change, as is often observed in the Far North. In addition, the fact that the desire for alcoholic beverages arises in psychologically difficult situations, if we consider mental conflict as a mediating factor in changing the physiological background, also indicates the role of physiological predisposition. It is known that alcoholism develops less often with diabetes, and more often with tuberculosis. A resected stomach, hypovitaminosis of the thiamine group, a state of exhaustion, and an existing dependence on sedative drugs contribute to the formation of alcoholism. The development of alcoholism is prevented by the state of mental stress and the hypomanic phase of manic-depressive psychosis.
The specified circumstances seem promising for a targeted search for the causes of the formation, in particular accelerated, drug addiction. The search for possible physiological prerequisites for alcoholism is carried out on animals. These studies were started by R. Williams (1947), who showed that changing the concentration of amino acids in the diet changes the attitude of animals towards alcoholic beverages. The fact of variations in the attitude towards alcohol in animals that have not previously tried alcohol due to changes in the diet (not only changes in the content of amino acids, but also fats, carbohydrates and mineral salts) can be considered proven.
Information about pathogenesis alcoholism are quite diverse, they include biochemical, functional, physiological and anatomical and morphological concepts. Insufficient differentiation of clinical material, a “total” consideration of alcoholics at different stages of the addiction process, led to the fact that individual researchers obtained mutually exclusive results. Thus, in alcoholics they find both an increase and a decrease in the blood levels of calcium, chlorides, magnesium, copper, iron, hypo- and hyperglycemia, hypo- and hyperadrenergy.
This difference in data from the point of view clinicians Now it's easy to explain. Now it can be argued that, for example, hyperadrenergy is characteristic of the first and second stages of the disease, hypoadrenergy - for the third stage. It should be taken into account that an increase in the tone of the sympathetic system in the first stage of the disease may be clinically undetectable, since it is compensated by overexcitation of the cholinergic system, which is still intact. In the second stage, a decrease in the tone of the cholinergic system allows hyperadrenergy to appear prominently both during functional tests and in biochemical studies.
Ignoring staging alcoholism and the fact that at each stage different, often clinically polar, states are possible (different degrees of intoxication, different phases of withdrawal syndrome, different states of remission), explains many of the contradictions in the results of laboratory studies of alcoholics.
However, some pathogenetic changes in alcoholism it shows a clear progression, seemingly independent of the various states of the alcoholic. This applies, for example, to an increasing deficiency of vitamin B1, nicotinic and ascorbic acids, and a decrease in the synthesis of amino acids.
Indisputable also progressive changes in organs: fatty infiltration of the liver with transition to cirrhosis, degenerative changes in muscle tissue, changes in nervous tissue leading to macroscopically visible atrophy, increasing hemodynamic disturbances in the brain - from increased capillary permeability to perivascular edema, from vasodilation to massive hemorrhages and ruptures vessels and a number of other lesions, which we will focus on when describing the particular somato-neurological pathology of alcoholism. All this leads to the fact that the mortality rate of alcoholics exceeds the mortality rate of a population similar in age and gender by 3-5 times.
Alcoholism is a multifactorial and polyetiological disease. Along with the specific effect of alcohol, social, psychological and individual biological factors play an important role in the etiology of alcoholism. At the same time, premorbid character traits are also important, which not only determine the motivation for the attitude towards alcohol, but also influence the rate of development of the disease. In most cases, the personality of a person suffering from alcoholism is immature, with insufficient social adaptation and difficulties in establishing interpersonal relationships. The presence of such personality traits is explained by both heredity and defects in upbringing. In order to compensate for their condition, such individuals often resort to drinking alcohol or other psychoactive substances.
The following social factors are identified that predispose to the development of the disease: society’s attitude towards drinking alcohol; attitude towards alcohol consumption of the dominant religion in society (tolerant or prohibitive); state alcohol policy (availability and level of consumption); drinking traditions and customs; ethnicity, marital status, level of education, etc. Very great importance in the development of alcoholism is attached to the microsocial environment, the presence of a certain “alcohol climate” in it. The traditions and customs that have developed in the family and immediate environment shape not only the attitude towards alcohol consumption, but also significantly shape the personality, making it more or less susceptible to the risk of developing alcoholism.
Among the psychological factors in the formation of alcoholism, such personality traits as increased anxiety and suggestibility, lack of persistent and serious interests, insufficient ability to adapt in society, poor tolerance of physical and emotional stress, low self-esteem, hedonistic attitudes with the desire for immediate pleasure, lack of social -positive attitudes, inability to organize your leisure time and others. The specific psychological mechanisms of alcoholism are different for different types of accentuation and psychopathy. In unstable, hyperthymic and hysterical individuals, drinking alcohol is an expression of a general craving for pleasure; in psychasthenics, it is a desire to reduce anxiety and tension; in excitable individuals, it is a way of emotionally reacting to troubles.
Individual biological factors in the formation of alcohol dependence are primarily determined by heredity. It has been established that the risk of developing alcoholism in first-degree relatives is 7-15 times higher than in the population; the risk of getting the disease in identical twins is 2.5 times higher than in fraternal twins; In adult male children born to alcoholic fathers, the risk of developing alcoholism reaches 67%. There are entire nations with extremely low tolerance to alcohol. It is believed that it is not alcoholism itself that is inherited, but a predisposition to it, and a high risk of its development if abuse begins.
Despite the indisputable evidence of the role of the genetic factor, it is extremely difficult to establish its contribution to the development of alcoholism in the entire population of patients with alcohol dependence. This is due to the fact that patients in hospitals whose disease progresses unfavorably are usually examined. The majority of people suffering from alcoholism do not seek medical help due to good adaptation and a relatively favorable course of the disease. Apparently, these groups of patients differ significantly in the influence of environmental and genetic factors on the formation of alcoholism.
Among the biological factors of alcoholism, an important role is played by residual effects of organic damage to the central nervous system, delays and deviations in somatosexual maturation, chronic and acute asthenizing diseases, neuroticism in childhood, as well as early introduction to low-quality strong alcoholic beverages.
The pathogenesis of alcoholism is complex and not well understood. Alcohol is believed to affect almost all neurotransmitter systems in the brain. Low doses of alcohol stimulate the dopaminergic and noradrenergic systems, which is accompanied by euphoria and general excitement. High doses cause the opposite effect - a decrease in dopaminergic and non-radrenergic neurotransmission and an increase in the inhibitory effects of GABA. Clinically, this manifests itself as motor retardation and general sedation. Chronic alcohol intoxication causes a variety of biochemical and neurophysiological changes in the body as a whole and in the brain in particular. However, which of them are a consequence of intoxication, and which lie at the basis of addiction, has not yet been established.
It has been suggested that the basis of mental dependence is neurophysiological changes - pathological activation of certain hypothalamic systems, called the “pleasure center”. According to Academician I.P. Anokhina, alcohol affects the catecholamine system, primarily dopamine mediation in the area of localization of the “pleasure center” (limbic system, brain stem formations). Alcohol intoxication leads to the release of dopamine from the depot, its excess amount accumulates in the synaptic cleft and causes a euphoric effect. As alcoholism develops, dopamine reserves in the depot are depleted. It has been found that during withdrawal symptoms the concentration of dopamine in the peripheral blood increases; The more severe the withdrawal syndrome, the higher the concentration of dopamine. Withdrawal syndrome is accompanied by a decrease in the sensitivity of catecholamine receptors.
In recent years, amino acids that are neurotransmitters (GABA, glycine) and neurohormones (vasopressin), which play a role in maintaining alcohol tolerance, have been studied.
Among the biological factors, the role of the endocrine system and the ratio of the secretion of prolactin and testosterone were noted.
When studying the role of various ethanol-oxidizing systems, the important role of the liver enzyme alcohol dehydrogenase was revealed, which promotes the oxidation of alcohol to the final products (water and carbon dioxide). The deficiency of this enzyme, which develops in patients with alcoholism as a result of severe liver dysfunction, leads to the accumulation of acetaldehyde in the blood, which has a toxic effect on the brain
Alcoholism is a chronic disease characterized by a combination of internal and mental disorders. The cause of alcoholism is systematic alcohol abuse. One of the forms of substance abuse. Typical signs of alcoholism are changes in tolerance to alcohol, a pathological desire for intoxication, and the development of deprivation syndrome.Stages of alcoholism:
There is no uniform classification of alcohol dependence. During the course of the disease, a number of stages are distinguished (A.G. Goffman, 1985).Stage 1 is diagnosed in the presence of a pathological craving for alcohol and loss of quantitative control.
Stage 2 is diagnosed in the presence of alcohol withdrawal syndrome (AAS):
constantly occurring AAS (only after drinking medium or large doses of alcohol);
constantly occurring AAS, not accompanied by the appearance of perceptual deceptions or pronounced affective disorders;
constantly occurring AAS, accompanied by the appearance of perceptual deceptions or severe affective disorders;
extensive hangover syndrome, combined with pronounced changes in the nervous system or internal organs, as well as the psyche, caused by alcoholism.
Stage 3 is diagnosed when resistance to alcohol decreases:
decreased resistance to the end of binge drinking;
constant decrease in stability;
"true" binges;
the presence of pronounced changes in the nervous system, internal organs or psyche (up to dementia).
Stage 4 is diagnosed in old age when the intensity of craving for alcohol decreases, periods of alcohol abuse decrease, and their duration decreases:
reduction in the duration of periods
alcohol consumption, their less frequent occurrence;
transition to episodic alcohol consumption with a sharp weakening or disappearance of desire for it;
refusal to drink alcohol.
Etiology of alcoholism:
The main factors in the likelihood of developing alcohol dependence are the frequency of drinking alcoholic beverages and their volume.Hereditary predisposition, manifested in the accelerated conversion of ethyl alcohol in the body, is of great importance. A certain personality type (psychopathy, increased suggestibility, lack of serious life interests, difficulties in establishing interpersonal contacts), individual characteristics of neurotransmitter and oxidative systems also play a role.
The main causes of alcoholism:
The main role in the causes of alcoholism belongs to changes in the functional activity of the neurotransmitter systems of the brain. Disturbances in the metabolism of endogenous opiates, as well as catecholamine formations, predominate. The result is the emergence of a craving for alcohol, changes in reactions to its introduction, as well as the development of deprivation syndrome (withdrawal).Damage to internal organs and the nervous system during alcoholism is associated with the toxic effects of acetaldehyde (a derivative of ethyl alcohol), deficiency of vitamins (especially group B), changes in the functionality of enzyme and oxidative systems, impaired protein synthesis, and a decrease in the immunobiological reactivity of the body.
Symptoms and consequences of alcoholism:
The symptoms of alcoholism include a number of syndromes.Their combination determines the stage of the disease. At different stages, tolerance to alcohol changes (increases or decreases), protective reactions disappear during an overdose of alcohol, the ability to systematically drink alcohol and distort its effects, and amnesia for the period of intoxication are noted.
Mental dependence is manifested by an obsessive desire for intoxication, mental discomfort in a sober state and improvement in mental functions in a state of intoxication. With the development of physical dependence, a physical (uncontrollable) need for intoxication, loss of control over the amount of alcohol consumed, withdrawal symptoms, and improvement in physical functions while intoxicated arise.
The consequences of chronic intoxication manifest themselves both at the neurological, internal and personal levels, as well as in social activities. The neurological consequences of alcoholism include acute brain, so-called discirculatory-toxic syndromes (epileptiform, Gaiet-Wernicke, cerebellar, striopallidal insufficiency, peripheral neuritis, atrophy of the optic and auditory nerves, especially when using surrogates).
The consequences of alcoholism for the body are damage to the cardiovascular system, respiratory system, stomach, liver and pancreas, kidneys, polyglandular insufficiency of the endocrine system, and decreased immunological reactivity.
Among the mental consequences are asthenia, personality psychopathization, affective disorders (mood fluctuations, depression and dysphoria with aggressiveness and suicidal tendencies, in advanced cases - dementia (dementia). A characteristic manifestation is the so-called alcoholic humor - flat, rude, tactless. They can psychotic states arise - acute (delirious, hallucinatory-paranoid syndromes) and chronic (hallucinosis, delusions of jealousy, Korsakoff psychosis states.
The life expectancy of patients with alcoholism is shortened by 15-20 years due to the increased incidence of internal organs (especially cardiovascular pathology), as well as injuries. Working capacity is progressively declining. The timing of the onset of the consequences of chronic alcohol intoxication depends not only on the duration of the disease, but also on the compensatory capabilities of the body’s functional systems.
The development of alcoholism is usually preceded by many years of domestic drunkenness.
Against this background, resistance to alcohol increases, sleep, appetite, and the sexual sphere suffer. The sedative effect of alcohol is reduced: both intoxicated and sober, increased vitality and motor activity, and high spirits remain. At the same time, the feeling of being full of intoxication and vomiting in case of an overdose still persist, but in the latter case there is no longer any disgust at the thought of alcohol. The first signs of dysphoria appear when elevated mood suddenly gives way to periods of irritability and conflict, which disappear when drinking alcohol. The desire to drink arises for no apparent reason, and there is no critical attitude towards drunkenness.
The course of alcoholism by stages:
Alcoholism occurs in several stages.1 (first) stage of alcoholism:
At the first stage, resistance to alcohol continues to increase. Sometimes it increases 4-5 times. From time to time there is a desire to become intoxicated. At the same time, patients do not perceive the desire for intoxication as unnatural. They regard it on the same level as the feeling of hunger or thirst. Due to increased resistance, the ability to take high doses daily develops. However, if it is impossible to drink alcohol, the craving for it is temporarily overcome. When taking small doses, on the contrary, the craving for alcohol increases sharply and becomes uncontrollable. There is no feeling of satiation with intoxication. Also characteristic is the disappearance of vomiting during an overdose, forgetting of individual episodes of the period of intoxication (palimpsests), and lack of criticism of one’s condition. There is no physical dependence during this period; the syndrome of intoxication consequences may be limited to asthenic manifestations, temporary dysfunction of internal organs and the nervous system.The duration of stage 1 (first) of alcoholism ranges from 1 year to 4-5 years, after which the disease passes into the second stage. It is characterized by a maximum increase in resistance to alcohol. Patients are able to drink from 0.5 to 2 liters of vodka per day. The sedative effect of alcohol disappears, only the activating effect is observed. Despite the fact that outwardly the behavior is orderly, instead of forgetting individual episodes of intoxication, complete amnesia is observed. At first, amnesia is observed only when taking high doses. Mental dependence is manifested by a violation of the organization of mental activity in a sober state, a sharp decrease in mood due to the inability to drink (irritability, aggressiveness, hot temper). The ability for mental work decreases. Physical dependence develops with an uncontrollable craving for alcohol dictating behavior. After drinking small amounts of alcohol, the craving for alcohol increases uncontrollably, which leads to the development of severe stages of intoxication. Behavior becomes unpredictable.
2 (second) stage of alcoholism:
The development of withdrawal syndrome, characteristic of the 2nd (second) stage of alcoholism, is the most important criterion for the onset of physical dependence. At first it occurs only after drinking high doses of alcohol, and later - after drinking medium and small doses. The time for the development of withdrawal varies individually; on average, it develops 8-12 hours after the last use of alcohol.Withdrawal syndrome:
Withdrawal syndrome is characterized by the development of hypertonicity, overexcitation and hyperfunction in various internal organs, mental and neurological spheres: exophthalmos, mydriasis, hyperemia of the upper body, pastiness, large hot sweat, tremor of the fingers, hands, tongue and eyelids, gray-brown, thick coating on the tongue, nausea, vomiting, loose stools, urinary retention, lack of appetite, insomnia, increased blood pressure, dizziness and headache, pain in the heart and liver. An increase in anxiety, restlessness at night, and a seizure may be harbingers of acute psychosis.Symptoms of withdrawal syndrome of maximum severity are accompanied by profuse sweat, insomnia, trembling of the whole body, choreiform hyperkinesis, clonus of the kneecaps and feet, severe ataxia, muscle cramps of the arms and legs, convulsive seizures with loss of consciousness. Hypnogogic auditory, visual and tactile hallucinations may occur, and sometimes episodic hallucinations with the eyes open. The mood is anxious-fearful or melancholy-anxious with a tinge of irritability. Attention is unstable, its concentration is impaired. Patients are confused about numbers and dates and are unable to reproduce the correct sequence of events. During this period, the desire for intoxication is extremely strong. The duration of withdrawal syndrome of no more than 2 days indicates its mild course; severe withdrawal lasts up to 5 or more days.
Further development of the disease quickly leads to the appearance of binge drinking. Taking small doses of alcohol causes an uncontrollable craving for intoxication: alcohol is consumed many times during the day, abstinence becomes more severe and is accompanied by an intense craving for alcohol. During a binge, the craving for alcohol forces patients to use its substitutes (in the absence of ethyl alcohol) and take things out of the house in exchange for alcohol. The duration of such periods increases as alcoholism develops, and the time of abstinence between them decreases. After withdrawal symptoms are lifted, the craving for alcohol may subside for some time until the next binge. The duration of periods of abstinence varies individually - from several days to several months (on average - about 2-3 weeks). As a rule, this depends on various social and everyday reasons. The onset of another binge can be associated both with accidental consumption of alcohol and with the appearance of a craving for intoxication.
The consequences of intoxication on the part of the nervous system are represented by neuritis, the appearance of blind spots on the retina, narrowing of visual fields, decreased hearing at certain frequencies, ataxic disorders, nystagmus, impaired accuracy and coordination of movements, and acute cerebral syndromes are also possible. When examining internal organs, damage to the cardiovascular system, liver, etc. is noted. Any disease affecting the nervous system, as well as trauma or surgery, can be complicated by acute alcoholic psychosis.
In the mental sphere, personality disorders predominate: loss of creative potential, weakening of intelligence, psychopathization, affective disorders. In addition, the human psyche is regularly traumatized due to conflicts over drunkenness. One of the main reasons for personality changes is the restructuring of the scale of values. The craving for alcohol comes first.
Another reason is the toxic effects of alcohol and its derivatives on the brain. The following features are characteristic: ease of affect, weakened control over emotions, instability of reactions. At first there is a tendency to sharpen some character features, then they smooth out. There is depletion of motivation and motivation, and a rapid loss of interest in any activity. However, personality disorders are dominated by changes in the moral and ethical sphere. Qualities such as a sense of duty, honesty, and affection disappear. They are replaced by deceit, selfishness, shamelessness, frivolity, and loss of interest in one’s appearance.
Quite soon, thinking becomes sluggish and passive, judgments become superficial, and alcoholic topics predominate in conversations. Attention and the volitional sphere suffer. Irritability, grumpiness, and loss of sympathy even for close people arise and dominate. A number of patients experience increased excitability, anger, and a tendency to aggression. Others are dominated by a constantly high spirits, flat alcoholic humor, a tendency to joke, boast, and impudence. In some cases, instability of interests and a tendency to antisocial behavior are characteristic. Sometimes hysterical manifestations with demonstrative behavior and pseudo-suicide attempts predominate. Delusional ideas of jealousy, expressed at first only in a state of intoxication, can later develop into persistent delusions, extremely dangerous for the patient and his loved ones. The duration of the 2nd (second) stage of alcoholism is individual and can range from 5 to 15 years.
3 (third) stage of alcoholism:
Then comes the 3rd (third) stage of alcoholism, which is characterized by a decrease in resistance to alcohol. At first, it develops only towards the end of an alcoholic excess, but then severe intoxication is achieved from taking very small doses, accompanied by stupor or viciousness and aggression. Binges of many days end in psychophysical exhaustion, followed by abstinence from several days to several months; binge drinking may be preceded by mood disorders with sleep disturbances and an uncontrollable craving for alcohol; systematic (daily) drinking in small doses may persist. Another manifestation of a change in the body’s response at this stage is considered to be a decrease in the activating influence of alcohol, which now only moderately equalizes the tone, as well as amnesia, which ends almost every intoxication. Symptoms of mental dependence are mild due to the presence of the gross mental changes described above.Physical dependence is characterized by an uncontrollable desire that determines the life of the patient. Lack of quantitative control combined with decreased tolerance often leads to fatal overdoses. Intense attraction is also manifested by a loss of situational control (indifference to the time and place of drinking, the company of drinking buddies, etc.), which is also associated with the loss of intellectual functions.
Withdrawal syndrome is long-term and difficult, it is represented mainly by autonomic disorders: lethargy, immobility, drop in cardiovascular tone, pallor, cyanosis, cold sweat, sunken eyes, sharpened facial features, muscle hypotonia, ataxic disorders (up to the inability to move independently) . Reversible impairments of memory and intelligence often develop.
The next stage is the occurrence of alcohol degradation. There is devastation of the psyche, loss of emotional range, primitive affects (cruelty, anger), the manifestation of which is mitigated only by a drop in excitability and impoverishment of will. Fluctuations in the emotional background often look like dysphoria rather than depression. The development of persistent euphoria with a gross decrease in criticism is possible. Against the background of intellectual-amnestic disorders, psychopathic-like manifestations are formed with phenomena of hysteria or aspontaneity, passivity, and loss of interests.
The consequences of intoxication are represented not only by functional, but also by organic damage to vital systems. In the mechanism of their development, not only toxic effects play a role, but also metabolic and nutritional disorders, nervous regulation, fermentopathy, etc. Neurological disorders become irreversible. Encephalopathy and polyneuritis are usually observed; approximately 1/5 of patients with alcoholism in the third stage suffer from epileptic syndrome; in some cases, acute Gaye-Wernicke syndrome, which is life-threatening, is possible. Alcoholic dementia can manifest as pseudoparalytic disorders. Chronic hallucinosis, alcoholic paraphrenia and delusions of jealousy are possible. The patient is not capable of independent productive activity, except under duress, and needs constant monitoring. At this stage of alcoholism, almost all organs and systems are affected, most often a combination of liver pathology and myocardial dystrophy is detected.
The course of alcoholism is characterized by varying rates of progression. Severe progressive alcoholism develops over 2-3 years. At the same time, personal changes are profound, sometimes irreversible, there is no improvement in condition, and social disadaptation is pronounced. Moderately progressive alcoholism develops over 8-10 years, and personality changes can be moderate. Long periods of improvement are possible, and a decrease in social and labor adaptation is often noted.
Low-progressive alcoholism develops very slowly, the third stage of the disease does not occur at all. Personality changes are hardly noticeable, remissions can last for many years, and social adaptation may be completely preserved. Alcoholism develops at a higher rate in women (early family and work maladjustment), adolescents (possibly malignant), and elderly people (with the onset of the disease after 60 years).
With alcoholism, improvements in the condition (remission) can be observed not only as a result of treatment, but also spontaneously. Their onset and duration largely depend on the relevance of abstinence from alcohol, the personal characteristics of the patient, and the course of the disease. Relapses are associated with the actualization of the desire for alcohol, mental trauma, and the patient’s desire to check the effectiveness of treatment. Patients are unable to switch to moderate alcohol consumption, although after a long remission, a relapse may not occur immediately after the first use of alcohol.
Damage to internal organs due to alcoholism:
The first and especially the second stages of alcoholism are characterized by moderately high blood pressure. There is a rise in blood pressure to 180-160/110-90 mm Hg. Art. usually on the 1st-5th day after alcohol abuse. Higher blood pressure level - 200-220/110-130 mmHg. Art. - characteristic of the predelirious period. In addition to increased blood pressure, patients experience tachycardia up to 100-110 beats/min, facial hyperemia, hyperhidrosis, trembling of the hands, eyelids, tongue, instability in the Romberg position, and poor coordination during finger-nose and knee-heel tests.The classic form of alcoholic myocardial dystrophy is manifested by pain in the heart area, especially at night, shortness of breath, palpitations, and interruptions in heart function. Typically, deterioration of the condition develops after leaving the binge and is combined with symptoms of withdrawal syndrome. The pseudo-ischemic form is characterized by severe pain, the development of an enlarged heart, a slight increase in temperature, frequent rhythm disturbances, and the development of circulatory failure. In the arrhythmic form, rhythm disturbances come to the fore: atrial fibrillation, extrasystole, paroxysmal tachycardia; in addition, shortness of breath and an increase in heart size are noted.
Pain in the heart area occurs at night or in the morning and is not associated with physical activity; it does not disappear with taking nitroglycerin. Patients themselves note a connection between alcohol intake and increased pain. An objective examination reveals expansion of the borders of the heart to the left, muffled heart sounds, and systolic murmur at the apex. With severe heart damage, congestive heart failure develops (shortness of breath, acrocyanosis, orthopnea, liver enlargement, edema).
Damage to the respiratory system during alcoholism is manifested by the development of laryngitis, tracheobronchitis, pneumosclerosis, and emphysema. Patients most often complain of a painful morning cough with scant sputum, especially after alcoholic excesses. The cough is accompanied by shortness of breath that does not correspond to the degree of physical activity. When examining the function of external respiration, obstructive disorders are noted. The incidence of pneumonia in people suffering from alcoholism is 4-5 times higher than in other people. In this case, the inflammatory process in the lungs is usually severe, with a tendency to abscess formation. The most common outcome of the disease is pneumosclerosis.
The pathology of the gastrointestinal tract in alcoholism is the development of chronic gastritis and enterocolitis. Chronic alcoholic gastritis is characterized by the development of pain of varying severity and indigestion. In the morning, vomiting is typical, rather scanty and not bringing relief. It is combined with a feeling of fullness in the epigastric region, belching and loss of appetite with severe thirst. Often there is complete damage to the entire gastrointestinal tract, when the symptoms of gastritis are combined with changes in stool (alternating constipation and diarrhea).
Chronic alcoholic pancreatitis:
The damaging effect of alcohol and its derivatives also affects the exocrine function of the pancreas. Among the causes of the development of pancreatitis in men (in the absence of primary damage to the biliary tract), alcoholism ranks first. Acute alcoholic pancreatitis is manifested by an attack of severe pain in the upper abdomen immediately after drinking alcohol. The pain is so intense that it is accompanied by motor excitement and can quickly become shingles. It is usually accompanied by repeated vomiting, which does not bring relief. When palpated, the abdomen is soft and painful in the upper half.Chronic alcoholic pancreatitis is characterized by constant pain in the upper abdomen and umbilical region, and indigestion. The pain intensifies after drinking alcohol and eating, is combined with a feeling of fullness in the abdomen, unstable stools, and sometimes vomiting can occur. Relapses and exacerbations clinically resemble acute alcoholic pancreatitis. In some cases, type 2 diabetes mellitus can develop, usually with a mild course.
Alcoholic hepatitis:
Alcoholic liver damage in the initial stages of the disease is characterized by protein and fat depletion. Alcoholic hepatitis then develops, which can result in cirrhosis of the liver. Alcoholic liver dystrophy is manifested by moderate hepatomegaly (enlarged liver). Sometimes after drinking alcohol there is a feeling of discomfort in the right hypochondrium. This process is completely reversible: complete abstinence from alcohol leads to normalization of the size and function of the liver.Alcoholic hepatitis can occur as acute alcoholic hepatitis or chronic hepatitis. Acute alcoholic hepatitis develops with long-term alcohol abuse. After taking large doses of alcohol, the patient’s appetite disappears, nausea and vomiting, pain in the epigastrium and right hypochondrium appear. There is a moderate fever, pain in the joints, muscles, and aches throughout the body. After 2-3 days, hepatic jaundice occurs. When palpated, hepatomegaly and pain in the right hypochondrium are noted. In some cases, acute alcoholic hepatitis leads to the development of acute liver failure. Chronic hepatitis in alcoholism is characterized by hepatomegaly, periodic hyperbilirubinemia, especially after taking large doses, and dysproteinemia. The outcome of chronic hepatitis is alcoholic cirrhosis of the liver. Its course is extremely unfavorable with continued alcohol intake and can quickly lead to the development of liver failure.
Characteristic of alcoholism is kidney damage - alcoholic nephropathy. In its acute form, it manifests itself as nephronecrosis after consuming significant amounts of alcohol. With the development of a recurrent form, the patient experiences transient hematuria and proteinuria. When an ascending infection occurs, the condition may be complicated by pyelonephritis. It must be remembered that hematuria and proteinuria develop with every prolonged binge. Patients with alcoholism experience a decrease in sexual function (“alcoholic impotence” in men, early onset of menopause in women). First of all, this is associated with alcohol damage to the endocrine glands, primarily the gonads (sex glands).
Alcoholic myopathy:
There are acute, subacute and chronic alcoholic myopathy. In all forms, muscle pain, swelling, and pain in a wide variety of localizations occur; numerous skeletal muscles are involved in the process. In severe cases, widespread necrosis of muscle fibers, myoglobinuria with kidney damage are observed.Damage to the nervous system due to alcoholism:
Among the lesions of the peripheral nervous system, paralysis of the radial nerve with the development of a “dangling hand” is noted, which occurs after another alcoholic excess. In some cases, clinical brachial anesthesia is observed, pain syndrome occurs during the recovery stage. The nature of these injuries is associated with prolonged ischemia as a result of compression (“garden bench paralysis” - the patient, in a state of intoxication, falls asleep deeply with his hands on the back of the bench).Alcoholic polyneuropathy:
Alcoholic polyneuropathy is usually more severe and often affects the lower extremities and may have a recurrent course. In the initial stages, as a rule, there is pain in the feet and calf muscles, a feeling of numbness in the feet and hands. Subsequently, a decrease in the sensitivity of the extremities develops in the form of “gloves” and “socks”, sometimes deep sensitivity suffers more. In the latter case, tendon reflexes disappear faster, coordination of movements is impaired, and a clinical picture of pseudotabes is observed. Unlike tabes dorsalis, it is characterized by pain when the calf muscles are compressed. Some patients may experience symptoms of damage to the peripheral nervous system such as mixed polyneuropathies with the addition of atrophic paresis.In chronic alcoholism, so-called tobacco-alcohol amblyopia may occur - atrophy of the optic nerves with a sharp drop in visual acuity similar to retrobulbar neuritis.
Alcohol damage to the central nervous system:
Symptoms of alcoholic damage to the central nervous system are varied. Among them are alcoholic encephalopathies, alcoholic psychoses (delirium, hallucinosis, alcoholic delusional psychoses, alcoholic depression, alcoholic epilepsy, dipsomania). However, some studies of the brain do not reveal brain atrophy with any long-term alcohol history.Alcoholic dementia:
Alcoholic dementia (alcoholic pseudoparalysis) develops in patients over 40-50 years of age, mainly in men. The course of alcoholic dementia generally corresponds to that of any form of dementia. Intellectual and amnestic disorders (memory and thinking), emotional instability, personal degradation, untidiness and uncleanliness develop and progress. Against this background, the presence of delusional psychoses (more often delusions of jealousy) is often noted. Alcoholic dementia can occur with the development of joint damage, tremors, weakened pupillary reactions, nystagmus and alcoholic myopathy. Sometimes a combination of dementia and alcoholic polyneuropathy occurs, but even without the latter, tendon reflexes in the legs may not be evoked. The course of alcoholic dementia can mimic progressive paralysis. Only a classic serological reaction can exclude it.Alcohol delirium:
Alcoholic psychoses belong to the group of external psychoses caused by chronic alcohol intoxication. Alcoholic delirium (delirium tremens, delirium tremens) occurs acutely, several hours or days after stopping alcohol intake. The initial period is characterized by insomnia, weakness, the development of individual illusions and hallucinations, episodes of delusional perception of reality against the background of anxiety, excitement, and timidity of patients.Then jaundice of the sclera, hyperemia and swelling of the face, tachycardia, fluctuations in blood pressure are noted, and the size of the liver increases. An elevated temperature is observed. The most consistent symptom is trembling of the hands, head or whole body. Increased sweating and nystagmus, the appearance of pathological reflexes, general hyperreflexia, ataxia, and muscle hypotonia are often encountered.
A typical alcoholic delirium usually lasts from 2 to 5 days. In this case, false orientation in the place and surrounding persons, and inaccurate orientation in time are observed. Hallucinations intensify. They can be either simple in content, purely visual, or complex - scenic, combined. Visual hallucinations are often united by a common content, usually of a frightening nature. They are changeable and intertwined with illusions, disorders of the body diagram (metamorphic writings). They can be macromanic (huge faces, animals, monsters) and micromanic (small creatures - classic “green little devils”) in nature. Patients express unsystematic delusional ideas of physical destruction, persecution, accusations, expressing the content of their visual hallucinations - the so-called hallucinatory delusions. Fear dominates, there may be bewilderment, sometimes euphoria occurs. The patient’s behavior corresponds to the content of his hallucinations and delusions: he defends himself, tries to escape, chases someone away and shakes off himself and the objects around him.
Insomnia and increased symptoms in the evening and at night are typical. During the day, on the contrary, there may be some weakening of symptoms. If you can distract patients from painful experiences, you can obtain some anamnestic information (usually incomplete). The exit from the state of psychosis is usually critical - after deep sleep through the asthenia phase. Recovery may also occur gradually, with the development of delirium or depression. Subsequently, patients retain more complete memories of painful experiences than of real events.
Atypical forms of alcoholic delirium may include oneiric components and individual mental automatisms. At the same time, delusional ideas can be largely systematized, and hallucinations can be predominantly auditory in nature. Atypical forms last longer. Reduced forms that last about a day (abortive delirium) may also occur. Sometimes the course of delirium becomes more severe with the addition of stages of professional and excruciating delirium. Occupational delirium occurs against the background of a severe somatic condition. In this case, patients perform monotonous scattered movements, reminiscent of professional ones. They accompany them with fragmentary comments of a professional nature, and false recognitions are often noted. Memories of this stage are practically not preserved.
The development of excruciating delirium is characterized by a lack of reaction to others and to speech addressed to the patient. Against the background of a general extremely difficult condition, barely audible incoherent muttering, weak, uncertain, sometimes convulsive movements of the hands are noted (patients feel, finger the edge of the blanket, shake something off themselves). There is an elevated temperature, aggravation of the disorders existing in the pre-delirium period, and the addition of pneumonia. The condition may be complicated by stupor and coma. The fatal outcome of delirium tremens in a hospital setting, according to various sources, ranges from 1 to 16%.
Alcoholic hallucinosis:
Alcoholic hallucinosis can be acute, subacute and chronic. It is characterized by the presence of multiple auditory hallucinations and delusional ideas of persecution, physical destruction, accusations, etc., against a background of anxiety and fear. The content of delusions is closely related to the content of hallucinations. Consciousness is not darkened. Acute alcoholic hallucinosis lasts from several hours to 1 month. Auditory hallucinations come from one or more “voices” that threaten, reprimand, order, tease the patient, or discuss unseemly acts committed by him in the past. Auditory hallucinations are quite often of a scenic nature. Delusional ideas are poorly systematized and vague. In the initial period of acute hallucinosis, significant motor agitation may be noted. Acute hallucinosis can occur in erased forms (acute hypnagogic auditory hallucinosis, acute interrupted hallucinosis, which last about a day), in atypical forms (with depression, short-term substupor, individual mental automatisms, delusions of grandeur or oneiric inclusions), as well as mixed forms - with pronounced delirium or delirious episodes.Subacute alcoholic hallucinosis can last from 1 to 6 months. It differs from the acute one in the lesser severity of fear and excitement. In this case, auditory hallucinations, delusions of persecution and depressive affect predominate. Recovery from acute and subacute alcoholic hallucinosis can be critical or gradual.
Chronic alcoholic hallucinosis lasts a long time - from six months to several years - and is characterized by the presence of stereotypical auditory hallucinations. The statements of the “voices” can be neutral, commentary, like an “echo of thoughts.” Patients get used to them to some extent. However, during the period of intensification of hallucinations, fear is noticeable. Agitation is rare and unpredictable behavior is possible. Sometimes delirium may be absent or, conversely, predominant. In a number of cases, true hallucinations are replaced by pseudohallucinations, and at the same time mental automatisms arise. The progression of the disease leads to the transition to paraphrenia and pseudoparalysis.
Alcoholic delusional psychoses:
Alcoholic delusional psychoses can occur as acute or chronic paranoid, alcoholic delusions of jealousy. Acute paranoid is characterized by pronounced fear, figurative delusions of persecution or relationship. The patient takes those in contact with him as pursuers, and any objects in their hands as weapons. In real conversations, he finds hints of his own imminent violent death. The patient’s actions are aimed at running away from danger, preparing for defense or attack. The duration of acute paranoid ranges from several days to several weeks, although an abortive course can also occur - up to a day. Chronic alcoholic paranoid is characterized by more smoothly manifested symptoms. There is an intensification of pre-existing delusional ideas of persecution or the emergence of delusions of influence and other mental automatisms.Alcoholic delirium of jealousy:
Alcoholic delusions of jealousy (alcoholic paranoia) begin gradually. Against the background of a depressed or embittered emotional state, delusional ideas of jealousy arise and are systematized. They are often hidden by the patient from others and are first expressed in the heat of a quarrel or during intoxication. Over time, painful statements lose their credibility. The delusion of adultery expands, extends into the past, and is complicated by ideas of persecution, poisoning, damage, as well as fictitious events and auditory illusions. The patient’s activities are aimed at obtaining evidence of his wife’s “infidelity” and punishing the “offenders.” Often it results in brutal aggression resulting in murder. The course of alcoholic paranoia is long, many years. There are periods of attenuation and resumption of symptoms, which are associated with the intensity of alcoholism and the patient’s living conditions.Alcoholic depression is characterized by anxiety, tearfulness, irritability, hypochondria, suicidal tendencies, feelings of inferiority, and worsening mood in the afternoon. Depression can vary in duration and intensity.
Alcoholic epilepsy:
Alcoholic epilepsy is no different in symptoms from idiopathic epilepsy. Seizures may occur during binge drinking or during abstinence. With prolonged abstinence from alcohol, they do not recur. Dipsomania, the so-called true binge, occurs at the 3rd stage of alcoholism, often against the background of chronic, erased mental pathology. The beginning is the appearance of anxious-depressive affect, dysphoria, sleep and appetite disturbances, and headaches. Over an individually variable period (from days to weeks), patients experience intense cravings for alcohol and consume it daily. The binge is interrupted suddenly due to the disappearance of the desire for alcohol or the emergence of an aversion to it.Alcoholic encephalopathies:
Alcoholic encephalopathies are characterized by the presence of mental and somatoneurological disorders, and the latter may predominate. There are acute (Gaye-Wernicke syndrome) and chronic (Korsakoff's psychosis) encephalopathies. All forms of encephalopathy are characterized by a pre-illness period of varying degrees of duration: from several weeks to a year or more; it is shortest in the hyperacute form - 2-3 weeks. This period is characterized by the development of asthenia with a predominance of adynamia, loss of appetite up to complete anorexia, and aversion to fatty and protein-containing foods. A fairly common symptom is vomiting, mainly in the morning. Heartburn, belching, abdominal pain, and unstable stools are often observed. Physical exhaustion increases.Sleep disturbances are typical for the prodrome state - difficulty falling asleep, shallow superficial sleep with vivid nightmares, frequent awakenings, early waking up. There may be a distorted sleep-wake cycle: drowsiness during the day and insomnia at night. More often, sensations of chills or heat occur, which are accompanied by sweating, palpitations, pain in the heart, and a feeling of shortness of breath, usually at night. In various areas of the body, usually in the limbs, skin sensitivity is impaired, and cramps are observed in the muscles of the calves, fingers or toes.
Gaye-Wernicke syndrome:
Gaye-Wernicke syndrome usually occurs in men aged 35-45 years. The beginning, as a rule, is delirium with scant, fragmentary, monotonous hallucinations and illusions. Anxiety and fear dominate. Motor excitation is observed mainly in the form of stereotypical actions (as during everyday or professional activities). From time to time, it is possible to develop short-term states of immobility with increased muscle tone. Patients may mutter something, shout monotonous words, while verbal contact with them is impossible. After a few days, a state of stupor develops, which can then turn into stupor, and if the course is unfavorable, into a coma. In more rare cases, the soporous state is preceded by an apathetic stupor.The deterioration of the mental state is facilitated by the worsening of somatic and neurological disorders. The latter are very diverse. Fibrillary twitching of the tongue, lips and facial muscles is often observed. Complex involuntary movements are constantly observed, among which trembling alternates with twitching, choreiform, athetoid and other types of movements. Muscle tone can be either increased or decreased.
Ataxia soon develops. Nystagmus, ptosis, strabismus, fixed gaze, as well as pupillary disorders (anisocoria, miosis, weakened reaction to light until its complete disappearance) and convergence disorders are determined. Quite often, polyneuritis, mild paresis, and the presence of pyramidal signs are observed; stiff neck muscles can be determined from meningeal symptoms. Patients are physically exhausted and look older than their years. The face is swollen. The tongue is crimson in color, its papillae are smoothed. An elevated temperature is noted. Tachycardia and arrhythmia are constant, blood pressure decreases as the condition worsens, and there is a tendency to hypotension (collapse). Hepatomegaly is noted, and diarrhea is common.
The hyperacute course of alcoholic encephalopathy is characterized by the fact that first severe forms of delirium (occupational or mussing) develop. Autonomic and neurological symptoms of the prodromal period increase sharply. Body temperature reaches 40-41°C. After one or several days, a state of stunned state develops, progressing to a coma. Death occurs most often on the 3-6th day.
As a result of acute alcoholic encephalopathy, the development of organic psychosyndrome is possible. In Gaye-Wernicke syndrome, mortality is often associated with the addition of concomitant diseases, usually pneumonia, to which these patients are prone.
Korsakoff psychosis:
Korsakov's psychosis (alcoholic paralysis, polyneuritic psychosis) is chronic. Quite common in women suffering from alcoholism. Clinically, this is characterized by impaired memory and attention, which leads to disorientation of patients in space. The third typical symptom is the filling of memory gaps with fictitious events. Amnestic disorders are characterized by a complete or partial lack of memory for current events (fixational amnesia), as well as memory for events that preceded the disease (retrograde amnesia lasting from several weeks to several years). At the same time, memory for distant events is preserved. The content of confabulations that arise in response to questions asked corresponds to the facts of everyday life.Neurological disorders characteristic of Korsakov's psychosis are polyneuropathies of the extremities. They are accompanied by sensory disturbances, varying degrees of muscle atrophy, and decreased tendon reflexes. Severe mental and neurological disorders are most often unrelated to each other. Neurological disorders pass faster than mental ones. Young and middle-aged people, especially women, show significant positive dynamics in response to treatment.
Alcoholic cerebellar degeneration is characterized by ataxia of standing and walking, ataxia in the legs with no or minimal involvement of the arms. Nystagmus and dysarthria are not observed in most cases. The disease progresses over several weeks or months, followed by a long, stable course.
Diagnosis of alcoholism:
The diagnosis uses data on alcohol abuse, the presence of a pathological desire for intoxication, altered resistance to alcohol, the presence of withdrawal syndrome, and personality changes. Characteristic disorders of the nervous system and typical damage to internal organs are important.The multisystem nature of the lesion allows doctors of any specialization to diagnose alcoholism. In later stages, diagnosis does not cause difficulties. In the initial stages, you can use laboratory methods for diagnosing alcoholism - biological markers of chronic alcohol consumption: increased activity of alcohol dehydrogenase (ADH) and the microsomal ethanol-oxidizing system; decreased aldehydrogenase (AlDH) activity; detection of hyperlipidemia, general hypercholesterolemia, hypertriglyceridemia; increased levels of cholesterol in the composition of high-density lipoproteins (HDL).
The fact of chronic alcohol intoxication is confirmed by the high and fluctuating activity of the enzyme complex glutamyltransferase (GGT), alanine aminotransferase (ALT) and aspartate aminotransferase (AST), alkaline phosphatase (the most common and significantly increased activity). GGT in combination with ACT). Fluctuations in activity indicate the intoxication nature of the deviations and make it possible to distinguish them from enzymopathies of the pathology of internal organs. With abstinence in the early period of the disease, enzyme activity returns to normal.
The formed pathology maintains high activity of GGT, ALT and AST for up to six months.
Alcoholic myocardial dystrophy is characterized by the following changes on the ECG: sinus tachycardia, supraventricular extrasystole, atrial fibrillation, changes in the T wave and S-T interval. In the first and early second stages of alcoholism, a shortening of the P-Q interval, an obliquely ascending displacement of the S-T segment, and a high pointed T wave in leads V2-V5 are characteristic.
From the second stage (with an alcohol history of more than 10 years), in addition to the described changes, an enlargement of the left ventricle, intraventricular conduction disturbances in the form of splitting and widening of the QRS complex are recorded, and a negative T wave may appear. Echocardiography reveals widespread changes in the myocardium, enlargement of the cavities of the heart. A study of blood circulation at the first stage reveals changes of the hyperkinetic type with an increase in cardiac output and a decrease in peripheral resistance; As the disease progresses, a hypokinetic type of blood circulation is observed with a persistent decrease in cardiac output.
With the development of acute alcoholic pancreatitis, in addition to typical clinical manifestations, changes in blood cells are characteristic: leukocytosis with a shift in the leukocyte formula to the left and acceleration of ESR. The level of alpha-amylase in the urine is increased. A biochemical blood test also reveals increased levels of alpha-amylase, lipase, trypsin, gamma globulins, sialic acids and seromucoid. In chronic pancreatitis, the described changes are characteristic of the development of exacerbations. In addition, there is a decrease in glucose tolerance when performing a standard test.
Acute alcoholic hepatitis leads to an inflammatory reaction of white blood: leukocytosis with a shift of the formula to the left, an increase in ESR. The content of bilirubin in the blood serum, AST and ALT are many times higher than normal values. Chronic alcoholic hepatitis is characterized by transient hyperbilirubinemia, dysproteinemia - hypoalbuminemia and hypergammaglobulinemia.
Alcoholic psychoses are diagnosed in the presence of chronic alcoholism and a clinical picture of psychosis, including the dynamics of symptoms. It should be remembered that alcoholism can layer or provoke the development of many mental illnesses, therefore, in each individual case a thorough psychiatric examination is necessary. The diagnosis of alcoholic encephalopathy is established mainly on the basis of the clinical picture and anamnesis. It is necessary to differentiate them from delirium, brain tumors, schizophrenia, and acute symptomatic psychoses.
Treatment of alcoholism:
Treatment of patients should be gradual and comprehensive. The treatment regimen for alcoholism includes three stages, each of which has its own goals. The tasks of stage 1 include eliminating the consequences of massive alcohol intoxication and stopping the withdrawal syndrome. At stage 2, it is necessary to achieve suppression of the pathological craving for alcohol and correction of psychological and internal disorders. Stage 3 - preventive therapy.For the treatment of withdrawal syndrome in combination with detoxification therapy (hypertonic, isotonic, plasma-substituting solutions, thiol derivatives), B vitamins, as well as C, PP, etc., and cardiovascular drugs are widely used; drugs that normalize sleep and reduce secondary cravings for alcohol - benzodiazepine tranquilizers (lorazepam, flurozepam, phenazepam, grandaxin, diazepam), sodium hydroxybutyrate, chlorprothixene.
In the first days of alcohol deprivation, psychosis may develop. Therefore, parenteral administration of neuroleptics - phenothiazines and butyrophenones - is widely used. Anticonvulsants are widely used - carbamazepine (Tegretol, Finlepsin), sodium valproate. Among nootropic drugs, Orocetam is most widely used. It should be used if somatovegetative disorders predominate in the clinical picture of withdrawal syndrome.
To stop withdrawal symptoms, you can use special acupuncture regimens, craniocerebral hypothermia, and hemosorption.
At the second and third stages of alcoholism treatment, sensitizing agents continue to be used - mainly disulfiram (Antabuse, Teturam, Aversan, Esperal). The effect of the drug is associated with the suppression of aldehydrogenase (AlDH) activity, which leads to the accumulation of acetaldehyde. This process begins no earlier than 12 hours after taking disulfiram and continues for several days. As a result, a pronounced disorder of the functions of internal organs and the nervous system develops, the so-called antabusalcohol reaction (AAR). This makes it impossible to take disulfiram and alcohol together. However, recently there has been a relatively low effectiveness of sensitizing therapy, both with disulfiram, which has a large number of side effects, and with other drugs (trichopolum, cyamide, furazolidone, nicotinic acid).
The most widely used drugs for the treatment of patients with alcoholism at the second stage are anti-thymoneuroleptic drugs (teralen, truxal, thioridazine, neuleptil). Antidepressants (tryptisol, pyrazidol, azaphene), which combine antidepressant and sedative effects, are widely used to treat depressive spectrum disorders. At the second stage of therapy, the use of benzodiazepine tranquilizers continues. However, it should be remembered that patients with alcoholism easily form cross-dependence, including to this group of drugs.
At the second stage, after the cessation of abstinence, the main goal of treatment is to create a stable improvement in the patient’s condition. This can only be achieved through the combined use of pharmacotherapy and psychotherapy. First, individual and then group psychotherapy is used, which have the greatest therapeutic potential. It allows patients to form a critical attitude towards the disease, as well as receive support not only from the doctor, but also from other members of the group.
At the stage of established remission in the interictal period, a course of therapy with psychotropic drugs may be required in cases of spontaneous deterioration of the condition or under the influence of unfavorable external factors leading to the resumption of pathological craving for alcohol at one time or another. Long-term contact with a psychotherapist (narcologist) or members of a self-help group is desirable to prevent the development of relapses.
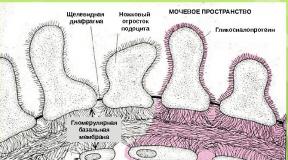
The central issue in the study of the pathogenesis of alcoholism is the establishment of its neurobiological mechanisms. In recent years, a lot of data have appeared on changes in the central nervous system, in particular dopamine and serotonergic structures, under the influence of ethanol, providing grounds for a partial revision of traditional approaches to understanding the pathogenesis of alcoholism. Easily absorbed from the gastrointestinal tract, ethanol quickly moves from the bloodstream to the brain, where it interacts with neurons. Intercellular membranes do not pose a significant barrier to ethanol, but its effect on cellular membranes has not yet been fully elucidated.
Membrane theory of the development of alcoholism
According to the so-called “membrane theory,” alcohol has a destabilizing effect on the membrane of nerve cells, increasing the “fluidity” of the membrane by changing the physical properties of its lipid components. But this theory allows us to explain only the effect of high doses of alcohol, which have a sedative and analgesic effect on the body, but the effects of small doses, in particular euphoria and the reduction of phobic experiences, remain unclear. There is evidence that these effects are due to the reaction of ethanol with specific receptive fields of cell membranes. These membrane-associated proteins respond exclusively to low concentrations of ethanol.
The effect of ethanol (acetaldehyde) on the human body
Acute ethanol intoxication is a consequence of the effect on the body not so much of alcohol itself, but primarily of its main metabolite - acetaldehyde. It increases the release of catecholamines from adrenergic endings, which increase the tone of muscular arteries and arterioles, cause tachycardia, and increase the need for oxygen in the myocardium and other tissues.
It also interacts with the GABAergic system and affects the functioning of calcium channels. By condensing with dopamine, acetaldehyde is able to form a substance - salsolinol, which provokes withdrawal symptoms, and condensation with serotonin leads to the formation of the MAO inhibitor harmaline, which is a powerful hallucinogen. These substances can accumulate in the neurons of the central nervous system, acting as “false mediators”, replacing catecholamines. They promote the release of endorphins and can themselves activate opiate receptors.
Other toxic effects of ethanol
Other toxic effects of ethanol (acetaldehyde) include:
- Inhibition of the elimination of ethanol metabolic products due to impaired liver function;
- Metabolic disorders due to suppression of redox processes;
- Accumulation of fatty acids, glycerol, pyruvic acid in the blood plasma and, as a consequence, the development of metabolic acidosis and pulmonary edema;
- Hypocalcemia and hypoglycemia, which can cause seizures;
- Capillary toxic effect;
- Increased platelet aggregation.
Chronic alcohol use
Chronic alcohol use is generally characterized by two main processes:
- Development of tolerance to alcohol.
- Alcohol addiction.
That is, in essence, the central nervous system and other organs seem to “learn” to react to the presence of alcohol in the body in such a way that each time an even larger dose of alcohol is required to obtain the expected (habitual) effect.
Development of tolerance to alcohol
Tolerance to the effects of ethanol is formed by various neuronal mechanisms:
- Vasopressin;
- Calcium ions through activation of the adenylate cyclase system;
- Neurotransmitters GABA, glutamate, serotonin and norepinephrine;
- Changes in the properties of the lipid bilayer and regulatory proteins of the plasma membrane;
- Receptors (NMDA).
It must be remembered that although the tolerance mechanism is capable of maintaining a high concentration of ethanol in the blood without pronounced signs of intoxication, the body still pays with significant damage to tissues and organs, primarily the brain, liver, pancreas, heart, and immune system.
Development of alcohol dependence
In the development of alcohol dependence, the reinforcing properties of ethanol, which are studied within the framework of behavioral theories, are of great importance. Knowledge of these mechanisms is quite important for understanding the effect of ethanol on the brain and the desire (often uncontrollable) for repeated drinking.
About positive reinforcement they say if an individual’s behavior is aimed primarily at obtaining pleasure (rewards).
At negative reinforcement- the dominant motive of all efforts is to avoid unpleasant sensations and discomfort. The euphoric effect certainly refers to positive reinforcement, and the state of anxiety reduction (anxiolytic effect) - to negative.
The emotional experience in a state of alcoholic euphoria is caused by the activation of the diencephalic-limbic structures of the brain, where areas of positive reinforcement (rewards) are localized. However, euphoria is obviously not only a consequence of the activation of positive reinforcement zones, but also the inhibition of negative reinforcement zones. That is why people in whom alcohol causes either pronounced euphoria or a reduction in emotional stress and anxiety are prone to alcoholism. In this case, the activity of the midbrain reticular formation is suppressed, which manifests itself in fear, anxiety, and a feeling of hostility from the environment.
Less studied are the neuronal systems involved in the formation of alcohol dependence. The role of the exchange of specific proteins and the mechanism of GABA-mediated chlorine ion current is assumed. With chronic alcohol consumption, GABA-mediated inhibition of nerve cells decreases, which can cause convulsive discharges in the hippocampus.
Other researchers believe that the reason for the formation of convulsive activity is an increase in sensitivity and an increase in the number of NMDA receptors under the influence of ethanol. As a result, sensitivity to glutamate increases and GABAergic activity decreases, and therefore nervous excitability increases, which characterizes the state of withdrawal. Because NMDA receptors are coupled to calcium channels, intracellular calcium levels may be critical to cellular excitation and the occurrence of seizures following ethanol withdrawal.
It has been proven that chronic alcohol intoxication activates voltage-sensitive calcium channels in the brain. Moreover, the acute effect of ethanol reduces the absorption of calcium, while the chronic effect, on the contrary, increases it as a result of cell adaptation processes.
Psychogenetic concept of alcoholism
According to the so-called psychogenetic concept of alcoholism by K. Blum and M.
Trachtenberg can schematically distinguish 3 types of alcoholic behavior, illustrated in the form of the following formulas:
- With a predominance of genetic predisposition factors: desire for alcohol (PA) = genetically determined deficiency of mediators, primarily opiate peptides + environmental factors (FOS);
- Triggered by stressful situations: PA = genetically inherited normal levels of neurotransmitters + deficiency of neurotransmitters and opiate peptides due to FOS;
- Associated with the toxic effects of alcohol: PA = genetically inherited normal levels of neurotransmitters + alcohol-induced deficiency of neurotransmitters and opiate peptides.
In the normal physiological state, which is characterized by a state of "opioid sufficiency", there is a balance between synthesis, release, binding to receptors and reuptake of the neurotransmitter, resulting in a feeling of inner comfort.
In a state of opioid deficiency caused by the above factors, some postsynaptic receptors remain unoccupied. This leads to cravings for alcohol, irritability, depression, fear and dysphoria. Acute exposure to alcohol leads to its increased metabolism and formation of tetrahydroisoquinoline, the so-called pseudotransmitters, which have the properties of agonists and antagonists of postsynaptic receptors and cause a deceptive feeling of comfort. At the same time, the natural synthesis of enkephalins decreases through feedback through the activation of presynaptic receptors of nerve endings. When ethanol consumption is stopped, the synthesis of enkephalins is restored rather slowly, but can be accelerated by appropriate pharmacotherapy.
Catecholamine hypothesis
Systematic alcohol consumption activates both the release and destruction of the mediator dopamine, which is a chemical precursor in the chain synthesis of adrenaline and norepinephrine, as well as the hormones of the sympathetic adrenal system themselves - adrenaline and norepinephrine.
Clinical manifestations of intoxication depend in a certain way on the content of catecholamines in the body: it is the excess content of released norepinephrine in the hypothalamus and midbrain that explains the phase of mental and motor excitation during intoxication, and psychomotor retardation after a drop in its concentration.
Systematic drinking leads to depletion of dopamine and norepinephrine reserves, which causes withdrawal symptoms, and since drinking alcohol allows you to “normalize” the state and brings a feeling of euphoria, a primary pathological craving for alcohol arises. Increased tolerance to alcohol is also, to a certain extent, associated with a compensatory increase in the synthesis of catecholamines, the destruction of which requires increasingly large doses of ethanol.
It has also been noted that in persons with sthenic character traits in premorbidity, in which the activity of dopamine-b-hydroxylase is high, alcoholism develops slowly, over 8-10 years. In persons with hysterical excitable traits in premorbidity, with low activity of this enzyme, alcoholism usually develops quickly, within 1-2 years.
According to this theory, distinguishing “mental dependence on alcohol” and contrasting it with “physical dependence” is unfounded, since they are based on identical neurochemical processes.
Serotonin hypothesis
The effect of ethanol on serotonin metabolism in the body is biphasic. First, serotonergic activity increases, which is accompanied by a euphoric effect, and later is noticeably suppressed.
This way we can explain the formation of a growing need for alcohol and emotional disorders during the withdrawal period. It has also been noted that in people who abuse ethanol, the level of serotonin in the blood is lower than usual.
It is possible that a certain group of patients with alcoholism consists of people with a genetic defect in the serotonergic system of the brain.
This is also confirmed by the fact that those who suffer from the so-called. familial forms of alcoholism, the level of tryptophan (an amino acid - a precursor of serotonin) is noticeably lower compared to patients who developed non-hereditary, late-onset alcoholism. They begin to abuse alcohol at a fairly early age and are prone to antisocial behavior and violent acts towards both themselves and others.
There is no single factor that is responsible for variation in individual risk for developing alcohol use disorders. Evidence suggests that alcohol abuse and dependence have a wide range of causative factors, some of which interact to increase risk.
Family history
It is well known that the offspring of alcohol-dependent parents are four times more likely to develop alcoholism.
Data from genetic studies, particularly in twins, have clearly demonstrated a genetic component to the risk of developing alcoholism. A meta-analysis of 9,897 pairs of twins from studies in Australia and the United States found that the heritability of alcohol dependence was more than 50% (Goldman et al., 2005).
However, a meta-analysis of 50 families, twins, and stepchildren found that the heritability of alcohol abuse was 30–36% (Walters, 2002). Whatever the actual heritability, these studies indicate that genetic factors can explain only part of the etiology of alcoholism.
Other variations account for environmental factors and their interaction with genetic factors. Although no single gene has been identified for alcohol dependence, a number of genes that determine brain function have been implicated (Agrawal et al., 2008).

Psychological factors
There is strong evidence that a number of psychological factors contribute to the risk of developing alcohol use disorders. Various theories have provided evidence for the importance of education in the development of alcohol dependence..
Alcohol, being a psychoactive drug, has properties that produce pleasure effects and the ability to alleviate negative moods such as anxiety.
Conditioned reflexes may also explain why people become especially sensitive to alcohol-related stimuli or cues, such as the sight and smell of a favorite drink, as these cues can lead to cravings for further drinking, including relapse after a period of abstinence. (abstinence) (Drummond et al., 1990).
Social learning theory also provides some explanations for the increased risk of excessive drinking and the development of alcoholism. People can learn from family members or peer groups as part of the process of modeling drinking patterns and expectations of the effects of alcohol.
Adolescents with strong positive expectancies (e.g., that drinking is enjoyable and desirable) are more likely to start drinking at an early age and to drink heavily (Christiansen et al., 1989; Dunn & Goldman, 1998).
Personality factors
The idea that people with addictive personalities are more likely to develop alcoholism is popular among some doctors, but it does not have strong research evidence. Often in patients being treated for alcoholism, it is difficult to separate the effects of alcohol on personality expression and behavior from those personality factors that preceded alcoholism.
However, people with alcohol dependence have a 21 times higher risk of having antisocial personality disorder (ASPD; Regier et al., 1990), and people with antisocial personality disorder have an increased risk of severe alcohol dependence (Goldstein et al., 2007). .
Recent evidence points to the importance of certain personality traits, such as adventure and novelty seeking and poor impulse control, as factors associated with an increased risk of alcoholism and drug addiction, which may have a basis in impaired brain functioning in the prefrontal cortex (Dick et al., 2007). ; Kalivas & Volkow, 2005).

Psychiatric comorbidities
People with alcoholism have higher rates of other comorbid psychiatric disorders, especially depression, anxiety, post-traumatic stress disorder, psychosis, or substance abuse, than people in the general population.
Alcohol can, at least temporarily, reduce symptoms of anxiety and depression, which has led to the theory that drinking in these situations is a form of “self-medication.” This theory lacks experimental support, and the long-term effects of alcohol worsen these disorders.
Stress, adverse life events and violence
There is compelling evidence that adverse life events can trigger excessive drinking and may predispose to the development of alcoholism. This is especially evident in alcohol dependence that develops after bereavement or job loss.
Stressful life situations or events can also trigger excessive drinking. People with alcohol dependence also report higher rates of childhood abuse, especially sexual abuse, and parental neglect.
One UK study found that 54% of women and 24% of men with alcoholism identified themselves as victims of sexual abuse, most before the age of 16 (Moncrieff et al., 1996). In addition, they were more likely to have a family history of alcohol abuse and began drinking and becoming dependent on alcohol at an earlier age than people without such a history.

Other environmental and cultural factors
There is a wide range of other environmental factors that predispose to the development of alcohol use disorders (Cook, 1994). These include the accessibility and availability of alcohol, high levels of alcohol consumption in the general population, occupational risk factors (such as working in the alcohol or hotel industry), social pressure, and religious and cultural attitudes towards alcohol.
Read also...
- Why do you dream about a man’s back?
- Fortune telling with hearts online: a simple and free way to tell fortunes about a guy’s love
- Dream Interpretation: flying above the ground in a dream
- Description of orange zest with photo, its calorie content; how to make it at home; use of the product in cooking; harm and beneficial properties