The structure of the uterus: where it is located, what it looks like, dimensions, pictures and photos with descriptions, anatomy of a woman (appendages, ligaments, cervix) nulliparous and pregnant. Determining pregnancy by touch Pregnant uterus in the early stages
During early pregnancy, the uterus initially does not change much in size, it only changes its shape and density. You can notice a change in the size of the uterus only by the 6th week of pregnancy, that is, after 2 weeks of delay.
Structure of the uterus
The uterus consists of a body, an isthmus and a cervix, which directly passes into the vagina. The highest part of the body of the uterus is called the fundus. It is the location of the uterine fundus that is one of the mandatory indicators that the gynecologist monitors at every visit to a pregnant woman, starting from the second trimester, in order to determine how the uterus is growing.
The uterus consists of three layers: the inner layer is called the endometrium, the middle layer is the myometrium, and the outer layer is the perimeter. The condition of the endometrium changes depending on the phase of the menstrual cycle. If the egg is not fertilized, then menstruation occurs, and the endometrium is released from the uterus, the mucous membrane is renewed. If a fertilized egg is implanted in the uterine cavity, the endometrium undergoes changes and thickens to provide nutrition to the fetus.
The myometrium is the muscular layer of the uterus. In the early stages of pregnancy, the uterus enlarges due to the active division of muscle cells. The myometrium grows and thickens, and after the 20th week of pregnancy, the growth of the uterus occurs due to stretching of the muscle fibers. The walls of the uterus in the second half of pregnancy stretch, and their thickness naturally decreases. Therefore, it is dangerous to become pregnant with a scar on the uterus due to a recent cesarean section or other gynecological surgery, for example, removal of uterine fibroids. After all, the scar becomes thinner along with the entire wall of the uterus and can separate.
Size and shape of the uterus
The uterus is pear-shaped. In the early stages of pregnancy, some “loosening” of the structure and ligaments of the uterus occurs so that it can actively grow and stretch. First, the uterus acquires a spherical shape, and then begins to increase transversely.
In nulliparous women, the uterus before pregnancy has a length of about 7 cm, a width of 4 cm and a thickness of about 4-5 cm. In women who have given birth, these dimensions may be slightly increased, and the weight of the uterus is 20-30 g more. Also, the size of the uterus increases, and the shape changes if there are neoplasms in it.
Pregnancy is already marked from the very beginning with signs of the presence of a fertilized egg. Changes primarily affect the reproductive organs. Therefore, it is natural that the cervix in the early stages of pregnancy, photos of which are given in the article below, changes. And the changes happening to her are one of the symptoms of the event awaiting the woman.
Location of the cervix in early pregnancy
Few women will be able, if necessary, to explain what this segment of the reproductive system is and what its significance is. This is easy to explain - it is impossible to monitor the problems or health of the cervix on your own. Its assessment and examination is the responsibility of the gynecologist conducting the examination.
This is the part of the organ visible during examination, which is transitional to the vagina, and also connects them. At each stage of the menstrual cycle, it produces mucus. At the same time, the role of the cervix in the early stages of pregnancy (see photo in this article) cannot be underestimated - it is it that largely ensures that the fertilized egg is kept in its proper place. Upon examination, only the vaginal part can be detected, although this is often enough to assess the state of health. When examined, it looks like a rounded formation protruding forward, having a small hole in the middle and covered with a mucous membrane.
The usual size of the organ is 4 cm in length and 2.5 centimeters in circumference, the pharynx is closed, the consistency is solid, and on critical days it becomes a little wider for the free release of secretions.
Changes in the cervix during early pregnancy are clearly visible to the doctor, which makes it possible to detect this condition. It is considered one of the main signs along with the cessation of menstruation.
Main functions
A woman's internal genital organs work smoothly if she is completely healthy. In normal condition, this organ performs several functions that help maintain the balance of microflora inside. Let's describe the main functions:
- favorable microflora is maintained thanks to the canal located in the vagina;
- there is mucus inside the pharynx that prevents all kinds of bacteria and microbes from entering the uterus;
- signals any changes that can be seen during examination;
- protects the fertilized egg from falling out;
- stimulates the reproductive organs to function normally.
It is difficult to overestimate the importance of this organ for a woman’s health. However, only an experienced specialist can read all the information.
Signs of cervical changes
So, let's figure out what the cervix is like in the early stages of pregnancy. It begins to change noticeably from about the fourth week, when the fertilized egg causes a slight protrusion of the wall, as well as an increase in the size and asymmetry of the organ. This can also only be detected by a specialist. Moreover, what kind of cervix is in the early stages of pregnancy primarily depends on how much time has passed since its onset. In this case, the increase in progesterone observed after conception leads to a visual change in the organ. This is easy to notice during a gynecological examination. An experienced doctor can accurately determine the period from the date of fertilization.

The cervix in the early stages of pregnancy acquires the following differences from its normal state:
- Its position changes significantly relative to the main part of the organ.
- The color of the mucous membrane acquires a bluish tint, which was pink before fertilization.
- When touched, the texture of the tissue becomes different.
There is no need to be afraid of such changes; they are caused by the activation of metabolic processes and the proliferation of blood vessels. This is necessary to improve blood supply, since the formation of the membranes of the fetus, in addition, its nutrition requires an increased amount of oxygen.
Changing the location of the vaginal cervix
When an embryo appears, the reproductive organs adapt to it in such a way as to provide it with comfort, normal development, and also protect it from possible dangers. This is what explains the changed position of the cervix in early pregnancy. It is not constant, changing at different stages of the cycle. But in general, this part of the organ is located quite high relative to the vagina. This is especially noticeable during ovulation - at this moment the body seeks to facilitate the penetration of sperm into the reproductive cell.
In the early stages of pregnancy, the cervix is low relative to its usual position. It is lowered by progesterone, thereby preventing the fertilized egg from falling out. depends on the level at which the cervix is located during early pregnancy - low or high.
If it is located high, this may indicate increased tone, which increases the risk of interruption. Due to this, some women have to spend almost the entire pregnancy lying down. But the doctor will take into account other signs. Probably, its high location is a feature of the body that does not threaten the fetus in any way.
Cervix consistency
The cervix in early pregnancy is soft to the touch compared to its previous state. This is explained by a significant dilation of blood vessels, more active work and swelling of the glands. Progesterone also plays a role, making the uterus itself and its endometrium thicker and looser. Although the neck is denser than the walls of the organ. It is a certain lock that protects the fetus. At the same time, she becomes more mobile.
Some people worry that if it is soft, it will not hold the fertilized egg. The fears have no basis, since its channel is significantly narrowed, and the tissues will still be elastic normally and difficult to stretch for a certain time. The glands begin to actively produce more viscous and thick mucus. A large clot called a plug appears in the cervical canal, which performs several functions:
- ensures the maintenance of microorganism balance;
- does not allow foreign bacteria to enter the uterine cavity;
- creates conditions for normal functioning of the reproductive organs.
If the cervix is too hard to the touch, this may indicate excessive tension in the organ (hypertonicity). This condition is dangerous due to the possibility of rejection of the fertilized egg. It is impossible to assess the consistency of the cervix on your own.

Therefore, there is no need to “wind up” yourself. Regular visits to the doctor are a guarantee that the pathology will be identified before it is too late to correct it.
Short neck
Not all women have a problem-free pregnancy. One of the most serious is the threat of interruption, caused by various reasons.
It is worth noting that the development of the fetus, in addition, its significant weight gain, increases pressure on the cervix. Sometimes it shrinks in size and can no longer be a full-fledged protection. This condition is most often caused by hormonal reasons, although it occurs with injuries received in the past by the organ, polyhydramnios and multiple births. This phenomenon is called "isthmic-cervical insufficiency." It requires medical supervision and treatment. Let us highlight the symptoms of cervical shortening detected by the doctor:
- excessive mobility;
- too soft consistency of fabrics;
- dilated lumen (the cervix is slightly open in early pregnancy).
For some girls, these signs are mild, but in any case she herself will not notice the problem, especially in the first weeks. The anomaly must be seen by a doctor, which requires mandatory registration, as well as a huge number of examinations.
The danger of shortening the cervix
Shortening the cervix during early pregnancy is dangerous due to the high risk of miscarriage. Isthmic-cervical insufficiency, instead of a very dense ring that protects the embryo from falling out, leads to the appearance of an element that provokes bleeding around it. This part of the organ cannot contain the increasing pressure, which leads to tone. The uterus becomes tense, hard, its muscles can begin to actively contract at any moment, trying to reject the fertilized egg.

This is dangerous at an early stage because the symptoms of cervical contraction during pregnancy are not always visible to the woman herself. Shortening of a section of this organ is detected using transvaginal ultrasound, prescribed at different times. At the same time, some girls experience:
- the cervix bleeds in early pregnancy;
- the appearance of watery discharge;
- nagging pain in the lower back, lower abdomen, discomfort in the form of tingling in the vagina;
- frequent need to urinate.
From time to time, the short length of this part of the organ can be congenital, most often it is an acquisition. Although, in order not to provoke shortening of the cervix itself and not create a threat to the child, a woman should take care of this even before pregnancy, in other words:
- do not smoke, as this bad habit provokes the development of hormonal disorders;
- avoid abortion;
- do not overwork and do not be nervous during pregnancy itself.
Cervical examination
In addition, with the help of mirrors, as well as two-handed examination, the gynecologist will refer the girl to undergo the necessary microflora analysis. You should make sure that there is no fungus or sexually transmitted infections in her body that could harm the fetus. We are talking about the microflora of the vagina, and it directly affects the general condition of the cervix.
The following cytology study allows us to study the normal structure of cells in a given area of the organ. At the same time, the cervix is not at all immune from their possible degeneration into malignant ones.
A changed cervix in the early stages is not just one symptom of an “interesting position.” In addition to protective functions, it informs about possible problems that can lead to a sad end if the right measures are not taken. Therefore, girls do not need to be afraid and avoid intravaginal ultrasound and gynecological examination, especially if there is a history of premature birth, miscarriage, or abortion.
Cervix is bleeding
If the discharge, which is a physiological norm, becomes brownish in color or includes inclusions of blood, there is a high probability that it is the cervix that is bleeding. This type of discharge is never associated with menstruation and is mostly spotty in nature.

Basically, the cervix bleeds due to existing erosion, which is small ulcers that secrete blood.
Damage to the mucous membrane is possible. They occur during sexual intercourse, in addition, during a medical examination, and this may also be accompanied by slight bruising of the cervix.
In addition, cervicitis (inflammatory processes), uterine polyps may also appear, sometimes the cause of the appearance of blood can be several of the above at the same time.
Early pregnancy: cervical discharge
In the first ninety days of pregnancy, the occurrence is not uncommon. They are observed in almost 20% of pregnant women. This process is not always associated with pathology. For example, the cervix may bleed at the very beginning of pregnancy, after the egg attaches to the uterine wall, if it has been successfully fertilized. Such discharge continues for about 2 days. In the 3rd trimester, the appearance of blood may already indicate that this requires prompt medical intervention.
Before starting treatment, you should find out exactly why the cervix is bleeding.

If erosion is the cause, the specialist will prescribe various healing medications, douching and herbal baths.
The main method of treating polyps, which cause bloody discharge from the uterus, is surgery.
Sometimes the appearance of blood occurs with cancer. In this case, a biopsy is mandatory.
Erosion
Already in the very first months, the expectant mother goes to the antenatal clinic for mandatory registration, where she undergoes all kinds of necessary medical examinations, and also prepares to meet her baby and the upcoming birth. Consequently, it is possible to identify various pathologies or diseases in a timely manner, in addition to preventing their possible complications. Cervical erosion is one of the most common and most frequently diagnosed diseases.
It is detected very often at the very first gynecological examination. The doctor examines the girl using a special mirror and also makes a smear for cytology. The pathology looks like a small defect located on the cervix, namely on the mucous membrane, in the form of an ulcer or redness.
In medical practice, pseudo- and true cervical erosion are distinguished. The pregnant woman then makes a note in her personal card about the presence of the pathology. This is done so that other specialists who will be present at the birth pay close attention to this.

It should be noted that cervical erosion in early pregnancy can be the result of various reasons. The very first of them is a violation of the girl’s hormonal background, which begins to change at the very beginning, right in the first trimester. In addition, the occurrence of cervical erosion is facilitated by all kinds of sexually transmitted infections (mycoplasma, chlamydia, gonorrhea) received by a woman before or during pregnancy, chemical and mechanical action, improper, rough douching, as well as many other factors.
In addition, the development of the disease is affected by frequent changes of sexual partners and decreased immunity.
Nature has provided all women with the amazing ability to bear and give birth to a child. For this purpose, the body has a special organ – the uterus. It is her condition that mainly determines the favorable course of pregnancy. If there is a pathology, it will be difficult for a woman to get pregnant, carry and give birth to a baby.
The health of this organ will be monitored by a gynecologist throughout pregnancy. How many times does the uterus stretch? What value is considered normal at different periods? What pathologies may occur?
A little about physiology: the structure of the uterus
The uterus is the main organ of the female reproductive system, with the help of which it becomes possible to bear a child. It is hollow inside and unpaired. The uniqueness of the uterus is that, thanks to its muscular structure, it stretches very much, and after childbirth it returns to its original state.
Due to the extensibility of the ligaments, the uterus can change its position in the woman’s body relative to neighboring organs. In the absence of pregnancy, it is located between the bladder and rectum, in the lower abdomen. Many people feel pain during menstruation, so they know exactly where it is located.
It is important to know the structure of the uterus. It consists of the body of this hollow organ and a narrow part - the neck. Doctors call the upper point of the uterus the fundus, and the isthmus is located between the cervix and the body. In its shape it resembles an inverted pear. The dimensions of the uterus outside pregnancy are small - length 7 cm, width 4 cm, and thickness 5 cm. In multiparous women, these parameters can be increased.
In section, the organ is divided into:
- endometrium or inner mucous membrane;
- myometrium, muscles;
- outer fabric.
What happens to the uterus during pregnancy?
Lack of menstruation is the first sign of pregnancy that you should pay attention to. If it does not occur, during menstruation the inner layer of the uterus is shed and bleeding and mucous discharge begin. Some women note a one-time onset of menstruation in the first month of pregnancy, which is associated with cycle disruption and late ovulation.
If fertilization occurs, the endometrium becomes thicker and softer, but the uterus itself does not yet increase in size. Only some swelling is noted due to changes in the inner wall. Subsequently, the fertilized egg attaches to the epithelium and the placenta is formed. Muscles and tissues become elastic - they are preparing for a big job.
A gynecologist or ultrasound specialist will be able to determine the onset of pregnancy in the early stages by external signs. During a chairside examination, the doctor assesses the condition of the cervix. Normally it is pink, but in a pregnant woman it takes on a bluish tint. This is due to intense blood circulation in this area. The same thing happens with the external genital organs - the blood flow increases, which means their color changes to a darker one. In the early stages, the cervix changes its position, descending (see also:). The structure of its tissue becomes more loose. The photo shows the appearance of the cervix in the early stages.

All changes in a woman’s reproductive system occur due to hormonal changes. The main “culprit” of the transformation is progesterone, the pregnancy hormone. It allows the uterus to bear a child by relaxing its muscles for nine months.
Based on these signs, the gynecologist will conclude about conception even without an ultrasound examination. The doctor will definitely palpate the organ and evaluate its mobility and softness. Non-compliance with standards may indicate a pregnancy pathology or disease. If the specialist still has doubts, he will prescribe additional tests and ultrasound. What the uterus looks like and its expansion at the beginning of term is shown in the photo.

Outwardly, there are no signs of pregnancy yet. The expectant mother often has no idea about her situation. The first symptoms of toxicosis will begin later, when the embryo attaches to the inner wall of the uterus, but for now it has just begun its journey through the fallopian tube. Some even feel the approach of menstruation, but it does not come.
This is the most dangerous time to continue pregnancy. Those who were planning to conceive should be very careful. Until the embryo attaches to the endometrium (first week), the probability of abortion is very high. Interestingly, in order to successfully adapt to pregnancy, the mother’s body reduces its own immunity, otherwise it will simply reject the fertilized egg.
When does it start to increase?
Indicators of uterine growth and its location are very important for assessing the health of the mother and baby. A noticeable increase in the organ occurs from about the fifth week. If before it looked like a pear, now it looks more like a round apple. During pregnancy, the uterus can be clearly felt through the abdominal wall as early as the third month.
The growth of the uterus is associated with the intensive development of the baby inside it. Its size increases very quickly, cells are actively dividing, and as a result, the belly of the expectant mother grows.
When does the uterus rise into the abdominal cavity?
Throughout pregnancy, the uterus grows and rises in the abdominal cavity, displacing neighboring organs. The highest position is observed three weeks before birth.
At each appointment, the doctor measures the height of the uterine fundus and determines how far it has risen into the abdominal cavity. In the second trimester, the uterus can already be felt without being examined on a chair - this is how gynecologists assess its condition. All parameters are strictly recorded in the patient’s medical record. It is important for a specialist to assess the dynamics of pregnancy. The expectant mother lies down on the couch, and the doctor uses a measuring tape to measure how high the uterus is in the abdominal cavity. A slight distortion can be caused by an unemptied bladder, so you need to go to the toilet before the examination.
What modifications of the uterus are considered normal?
During pregnancy, the following indicators of uterine growth are considered normal:
- from the first month the shape changes - it becomes rounded and increases in width;
- at the initial stages, noticeably asymmetrical development - one side is larger than the other (this is due to the place of attachment of the embryo);
- when the baby completely occupies the uterus, the shape is smoothed out;
- from the second trimester, the uterus already leaves the pelvic area and fills the peritoneum;
- by the 8th month, the uterus reaches the ribs, it puts pressure on the gastrointestinal tract, complicating normal breathing (this is its maximum position);
- before childbirth, the baby’s head drops (and with it the uterus), the woman feels relieved.

Table of normal sizes of the uterus and its location by week (for a singleton pregnancy):
| Week of pregnancy | Length in mm (+/- 10 mm) | Width (+/- 10 mm) | Height of the uterus relative to the pubic line, cm | Position of the uterine fundus |
| 8 | 70-80 | 40-50 | 8-9 | Bottom below pubic line |
| 10 | 100 | 60 | 10 | Ascends to the pubic line |
| 12 | 120 | 70 | 11 | Reaches the pubic line |
| 16 | 140 | 80 | 14 | The organ is located between the navel and pubis |
| 18 | 180 | 90-100 | 16-18 | 6-7 cm above the pubic line |
| 20 | 200 | 110-120 | 18-20 | The fundus of the uterus is located 2 fingers below the navel |
| 22 | 210 | 120-140 | 21-24 | Almost reaches navel level |
| 24 | 230 | 140-160 | 23-26 | Raises to the level of the navel |
| 26 | 250 | 160-170 | 25-28 | Rises just above the navel |
| 28 | 280 | 170-180 | 26-30 | 2-3 fingers above the navel |
| 30 | 310 | 180-190 | 28-31 | Rises closer to the bottom of the sternum |
| 32 | 320 | 190-200 | 30-33 | Midway between the navel and costal arches |
| 34 | 330 | 200-205 | 31-34 | The bottom is located 14 cm above the navel |
| 36 | 340 | 210-220 | 33-36 | Located on the line of the costal arches |
| 37 | 350 | 220-230 | 35-38 | The uterus descends and begins to put pressure on the stomach |
| 38 | 350-360 | 230-240 | 35-37 | Drops a few centimeters |
| 40 | 370-380 | 250-260 | 32-35 |
When a woman is carrying two or more children, the normal parameters for her will be different. In addition, each patient and her child have individual characteristics that affect the course of pregnancy. This often depends on genetics. An experienced gynecologist will definitely take these characteristics into account before drawing conclusions about the normal size of the uterus.

You should consult your gynecologist about the condition of your uterus. Each pregnancy is individual and depends on many factors. Only a specialist will give a complete answer to concerns about bearing a child. A woman in this position is very vulnerable; any careless statement can lead to hypertonicity and the threat of miscarriage.
Woman's sensations and uterine growth
Usually the woman does not experience any pronounced sensations. The uterus grows gradually and painlessly. At the first stage, when the embryo has just attached to the endometrium, the woman may feel some tension in the lower abdomen. It occurs due to stretching of the ligaments that hold the uterus. Some people attribute nagging pain to approaching menstruation, because they are very similar. This tension especially often worries first-time women. Experienced mothers, as a rule, do not feel this.
Minor pain is normal only during the first month of pregnancy. Subsequently, they may indicate increased uterine tone, which must be treated urgently, otherwise a miscarriage will occur. Normally, the organ should be relaxed, which does not always happen. Hypertonicity is the subject of close monitoring by gynecologists.
The growth of the uterus causes discomfort to the expectant mother after 4–5 months. It becomes difficult for her to take a comfortable body position and fully relax. Many people complain of pressure from the uterus on the digestive organs. This causes heartburn, bloating, increased gas formation and nausea.
The rectum also suffers from an enlarged organ, which often leads to constipation. In the last stages, the expectant mother develops breathing problems due to pressure on the diaphragm, she feels shortness of breath.
In the second trimester, most women notice a change in their gait. This is due to a shift in the body's center of gravity. They begin to walk, leaning their torso back a little, spreading their legs wider. After giving birth, this feature will go away, it’s just that now it’s more convenient for a pregnant woman to maintain balance.
Women who have a scar on the uterus may experience discomfort. They describe them as a tingling or dull ache. The scar occurs due to cesarean section or other surgery. The danger is that the uterine tissue becomes thinner, and along with it the suture. The condition of the scar must be monitored throughout the pregnancy, otherwise it may rupture. In this case, minutes count; there is a direct threat to the life of the mother and child.
A pregnant woman should tell her gynecologist about any painful sensations in the abdominal area. The doctor will determine the source of the pain or refer you for additional examination. Sharp pain and bleeding indicate miscarriage (early term) or premature birth.

What conditions are considered pathological?
Pathological conditions of pregnancy are accompanied by:
- periodic abdominal pain resembling cramps (may radiate to the lower back);
- bleeding - even a small amount of blood indicates a serious disorder;
- unnatural discharge from the genitals (bloody, purulent, having an unpleasant odor, unusual consistency);
- dizziness, loss of consciousness;
- petrification of the abdomen (often accompanied by pain);
- swelling of the limbs;
- very rapid weight gain.
Most of these symptoms require calling an ambulance and urgent hospitalization. We are talking about the threat of miscarriage or premature birth. This is dangerous not only for the fetus, but also for the life of the expectant mother.
What pathologies may indicate uterine disorders:
- increased muscle tone (often leads to miscarriage);
- short cervix, when the organ cannot hold the embryo;
- inflammatory diseases of the reproductive system;
- polyhydramnios;
- cervical erosion;
- fibroids (characterized by organ enlargement);
- failure of the existing scar;
- displacement of an organ due to inflammation or adhesions.

The photo shows cervical erosion. If there is no threat of miscarriage, the mother will be prescribed outpatient treatment or given a referral to a day hospital at the antenatal clinic. The doctor will examine the patient daily and administer medication. At this time, a sick leave certificate must be issued. There is no need to give it up - overexertion and excessive activity now will not lead to anything good. A woman needs to be provided with peace, good nutrition and the absence of stress - only then is a normal pregnancy possible.
The female body amazes with its uniqueness not only externally, but also from the inside. Conception of a new life, development and birth of a child - all these tasks are performed by the main female reproductive organ. In it, the growing fetus spends the important and responsible nine months of its life. Not only the developmental characteristics, but also the viability of the baby depend on the health of this organ. You will learn detailed information about what changes occur in the uterus during pregnancy, as well as about possible pathologies of the organ from this article.
Uterus during early pregnancy
Let's start with the fact that from the first days of conceiving a baby, a woman's body experiences revolutionary changes. However, the uterus itself in the early stages of pregnancy remains without any special modifications, which cannot be said about its cervix. As a rule, it is in this place that significant restructuring occurs first.
So, immediately after fertilization, the uterine cervix changes its color. If before pregnancy it had a predominantly light pink color, then after the birth of a new life, the cervix becomes darker, acquiring a lilac color. This is explained by the fact that after conception, blood flow in the main reproductive organ of the female body increases, small vessels dilate, changing the color of the cervix.
When such a pathology occurs, a woman feels pain in the lower back or lower abdomen, which intensifies when walking, changing body position, and also when turning the body. In this case, pain may occur depending on the place in which the egg is attached. As the egg grows, the pain intensifies, and, as a rule, it is they that make it possible to determine the presence of a pathological pregnancy in a woman. For example, in cases where the egg is attached to the ampullary part of the fallopian tube, pain appears approximately in the eighth week of pregnancy. When the fetus is implanted in the isthmus, a woman may begin to feel pain as early as the sixth week. In case of ovarian or abdominal ectopic pregnancy, there are no symptoms of pathology during the first month. When a cervical pregnancy occurs, when the egg attaches to the cervix, pain is extremely rare, as a result of which the ectopic development of the embryo often goes unnoticed. That is why, if your period is late, it is very important not only to take a pregnancy test, but also to be examined by a gynecologist.
Now you know what changes the main reproductive organ of a woman undergoes during pregnancy. We hope that our information will be useful to you. And finally, we would like to wish you a happy pregnancy and an easy birth.
Especially for - Nadezhda Vitvitskaya
viewing
Updated:
Diseases of the uterus occupy one of the leading positions among all female pathologies. Their prevalence leads not only to a decrease in a woman’s fertility, but also to a disruption in the quality of life, as well as significant economic costs associated with the costs of diagnosis, treatment and forced absence from work.
The prevalence of uterine pathology is determined by its connection with other organs and systems and the structural features of the entire reproductive sphere.
Structure and dimensions
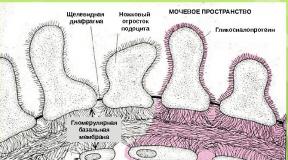
The uterus is an unpaired female reproductive organ, predominantly consisting of multidirectional smooth muscle fibers, externally covered with modified peritoneum (perimetry), and internally lined with mucous membrane (endometrium).
The adult uterus of a nulliparous woman is pear-shaped and flattened in the anteroposterior direction. Anatomically there are three parts:
- The fundus is the upper portion located above the line of entry of the fallopian tubes into the uterine cavity.
- The body is triangular in shape. The wide part of the body is directed upward, towards the abdominal cavity.
- The cervix is a direct continuation of the body of the uterus. There are two sections in the cervix:
- Vaginal region (exocervix), lined with stratified squamous non-keratinizing epithelium.
- Supravaginal area (endocervix, cervical canal, cervical canal), consisting mostly of smooth muscle fibers, surrounding the cervix in a circle, with inclusions of collagen and elastin fibers. The endocervix is lined with single-layer columnar epithelium.
This is what a healthy uterus should look like in a non-pregnant woman. When pregnancy occurs, the shape begins to change. In late pregnancy, the uterus looks like a spherical muscular formation with thin walls. In some cases, palpation and ultrasound examination in the early stages of pregnancy reveal its slight asymmetry. This is a variant of the norm and does not entail any consequences.
During pregnancy, the size of the uterus also changes. By the end of the second month of pregnancy, the size doubles, and by the end of the third month it quadruples.
Schematically, a woman’s uterus can be depicted as a triangle, the corners of which are the openings of the fallopian tubes and the cervix.
The shape of the cervix differs between women who have given birth and women who have not given birth. The cervical canal in nulliparous women resembles a spindle (that is, it is narrowed at the ends and widened in the middle), and the uterine os (the border between the cervical canal and the vagina) has a round or oval appearance. In women who have given birth, the cervical canal has a uniform width throughout, and the pharynx is a transverse slit with torn healed edges.
The size of the uterus can vary depending on the period of a woman’s life and the number of pregnancies and births she has had. According to ultrasound data, three sizes of the body and cervix are determined.
Location
The location of the uterus is the small pelvis, where its anterior wall is adjacent to the bladder, and its posterior surface is in contact with the rectum.
The uterus has a certain degree of mobility, and its position depends on the level of fluid in the bladder. If it is empty, then the fundus of the uterus is directed towards the abdomen, and the anterior surface is directed forward and slightly downwards. In this case, the uterus forms an acute angle with the cervix, open anteriorly. This condition is called anteversion. As the bladder fills, the uterus begins to tilt posteriorly, forming an angle with the cervix that is close to the unfolded one. This position of the uterus is called retroversion.
Functions
The only function of the uterus is to participate in pregnancy and childbirth. Due to its predominantly muscular structure, the uterus during gestation is capable of increasing its area several times. And thanks to the intense coordinated contraction of muscles during childbirth, the uterus plays a decisive role in expelling the fetus.
Anatomy
The wall of the uterus has a three-layer structure:
- The inner mucous membrane is the endometrium. Lining the inside of the uterus, the endometrium has no folds, is lined with ciliated epithelium and is rich in glands. The epithelium is also well supplied with blood, which explains its sensitivity to injury and inflammatory processes. In photos and videos taken during hysteroscopy, the inside of the uterus is a flat, smooth space of various colors - from pink to grayish, depending on the phase of the female cycle and the woman’s age.
- The middle muscular layer is the myometrium. This layer consists of smooth muscle cells intertwined in all directions. Because the muscle cells are smooth, the woman is unable to regulate uterine contractions. The consistency of contraction of various sections of the myometrium at different periods of the cycle and during childbirth is subject to the autonomic nervous system.
- The outer layer is the perimeter, which is the peritoneum.. This serous membrane covers the entire anterior wall of the body, and at the border with the neck it bends and passes onto the bladder. Here the vesico-uterine space is formed. The cervix in front is not covered by the peritoneum and is delimited from the bladder by a layer of fatty tissue. In addition to the entire posterior surface of the body, the peritoneum covers a small area of the posterior vaginal vault. After this, the membrane bends and spreads over the rectum, forming a rectal-uterine pouch. Fluid can accumulate in this space due to ascites. Purulent inflammation, endometriosis or malignant tumors can spread here. Through the posterior wall of the vagina, access is made to this space during a diagnostic procedure - culdoscopy.
Purpose of ligaments
The uterus is an organ for which a clear, relatively constant position is of fundamental importance. This is achieved through the ligaments of the uterus.
The ligamentous apparatus performs three main functions:
- Suspension – attachment of an organ to the pelvic bones in order to fix the uterus in a stable position.
- Fixing – holding the uterus in a physiological position during gestation due to tensile ligaments.
- Supportive – forming support for internal organs.
Characteristics of the hanging apparatus
The suspension function of the uterus is carried out thanks to four pairs of ligaments:
- Round uterine ligaments, containing smooth myocytes and connective tissue fibers. In appearance, they resemble cords 100–120 mm long, running from the corners of the uterus to the inguinal canal. Thanks to this direction, the round ligaments tilt the fundus of the uterus anteriorly.
- Broad uterine ligaments, which are derivatives of the peritoneum. They look like a “sail” stretched from the side surfaces of the uterus to the walls of the pelvis. At the top of these ligaments lie the tubes, and on the posterior surface are the ovaries. The space between the two leaves is filled with fiber in which neurovascular bundles are located.
- Suspensory ligaments of the ovaries, which are part of the broad uterine ligaments. They originate from the uterine tubes and are fixed to the walls of the pelvis.
- Own ovarian ligaments, which fix the ovary to the lateral surface of the uterus.
Structure and location of fixing ligaments
The fixing ligaments of the uterus are:
- Cardinal (transverse) uterine ligaments, which are powerful bundles rich in vessels and nerves, consisting of smooth muscles and connective tissue fibers. These ligaments are modified, strengthened broad ligaments for which the transverse ligaments serve as support.
- The uterovesical (cervicovesical) ligaments are muscle-connective tissue fibers originating from the cervix and encircling the bladder. Due to this direction, the ligaments prevent the uterus from moving in the posterior direction.
- The uterosacral ligaments are composed of smooth muscle and connective tissue fibers starting from the posterior wall of the uterus, wrapping around the rectum and attaching to the sacrum. These fibers prevent the cervix from moving towards the pubis.
Supporting apparatus: muscles and fascia
The supporting apparatus of the uterus is represented by the perineum - the muscular-fascial plate. The perineum includes the genitourinary and pelvic diaphragms, consisting of two layers of muscles, as well as the perineal fascia.
Structure of the ovaries
The ovaries are paired glandular organs located in the female body on both sides of the uterus and connected to it by the fallopian tubes.
The shape of the ovaries resembles an egg flattened in front. The mass of this organ is approximately 7 - 10 g, length - 25 - 45 mm, and width - about 20 - 30 mm. The color of a healthy ovary can range from pinkish-blue to blue-purple.
On the outside, the ovary is covered with coelomic (germinal) epithelium. Beneath it lies the fibrous tunica albuginea, which forms the framework of the ovary. The functionally active substance of the organ, the parenchyma, is located even deeper. It consists of two layers. On the outside there is a cortical layer in which the follicles are located. The inner layer - granular (medullary substance) contains the egg.
In addition to the maturation of eggs, the ovaries perform a hormonal function, synthesizing estrogens (estradiol, estriol), gestagens (progesterone) and testosterone.
The fallopian tubes
The uterine (fallopian) tube is a paired hollow muscular organ that connects the uterine cavity with the ovary.
The fallopian tubes range in length from 100 to 120 mm. The diameter of the pipe is different along its entire length and varies from 2 – 5 to 8 – 10 mm.
The fallopian tube contains the uterine part, which communicates with the uterine cavity, as well as the isthmus, ampulla and infundibulum.
The funnel contains fimbriae. The longest of them, the ovarian one, approaches the tubal end of the ovary. This fimbria guides the egg into the tube.
Endometrial polyps- benign proliferation of blood vessels covered with epithelium. There are several types of polyps:
- fibrous - pale, round or oval, dense, smooth formations on a stalk, up to 15 mm in size;
- glandular-cystic - large (up to 60 mm), oblong, smooth, pale pink, gray-pink or yellowish;
- adenomatous - dull gray formations up to 15 mm in size.
Polyps may be asymptomatic or cause bleeding, pain and infertility.
Prolapse of the reproductive organ
Prolapse (loss) of the female reproductive organs- this is the movement of the vagina, cervix or uterine body outside the genital opening.
There are three degrees of genital prolapse:
- I degree (not true prolapse): the cervix prolapses, but it does not extend beyond the entrance to the vagina;
- II degree: incomplete prolapse - movement of the cervix beyond the border of the genital fissure, but the uterus is in the pelvic cavity;
- III degree: complete prolapse - the entire uterus falls out.
The main cause of uterine prolapse is dysfunction of the ligamentous apparatus. This can be caused by connective tissue dysplasia, inflammatory diseases, and impaired innervation and blood supply to the genital organs.
At the first stage of prolapse, there may be no complaints. Sometimes women note a feeling of heaviness in the perineum, discomfort when walking, pain in the lower back and sacrum.
The most characteristic symptom of the second and third stages is a formation that has fallen outside the genital slit.
Upon examination, the prolapsed parts of the cervix and body of the uterus have a bluish tint. The reason for this is poor circulation in the prolapsed areas of the organ.
Conservative management of prolapse of the female reproductive organs is impossible! The only way to treat this pathology is surgery.
The operation is aimed at returning organs to their physiological location, restoring and strengthening the supporting structures of the uterus and treating associated pathologies.
"Uterine rabies"
This term hides two diseases that belong more to the field of pathological psychology than gynecology.
Nymphomania (“wood nymph disease”)– female hypersexuality, excessive attraction to men. This disorder is manifested by constant sexual dissatisfaction and the desire to constantly change sexual partners.
Hysteria (“the monkey of all diseases”) is a disorder characterized by a pathological need to attract attention to oneself. Although this condition also occurs in men, it is most pronounced in women. Hysteria can manifest itself with almost any known symptoms - uncontrollable laughter and/or crying, convulsive seizures, fainting, blindness, deafness, muteness, loss of sensitivity. It is not difficult to distinguish hysteria from a true disorder. It is enough to remember that hysteria manifests itself only in the presence of people whose attention the patient is trying to achieve.
Both nymphomania and hysteria require treatment from a psychiatrist and psychotherapist. But sometimes these disorders reach such severity that they require differential diagnosis with diseases of the nervous system (epilepsy, damage to the frontal lobes of the brain, stroke).
"Dense uterus"
A dense uterus is not an independent disease, but a symptom that accompanies the development of many pathological conditions. Uterine thickening means focal or total thickening of its walls, identified during a gynecological examination. The most common causes of the development of a dense uterus are myomatous nodes and foci of adenomyosis.
Adenomyosis (internal endometriosis) is a benign disease, which is based on the growth of the endometrium into the muscular layer of the uterus. The main symptoms to suspect adenomyosis are menstrual irregularities, intense dull pain in the lower abdomen, pain during sexual intercourse, and “chocolate”-colored discharge in the middle of the cycle.
If during the examination the gynecologist reveals a hardening of the uterus, an ultrasound should be performed to identify the cause.
Removal of the uterus and postoperative period
Indications for removal (amputation, extirpation) of the uterus (hysterectomy) are large myomatous nodes, malignant tumors of the uterus, widespread adenomyosis, heavy uterine bleeding, and severe inflammation of the endometrium.
With a favorable outcome, it is possible to save the ovaries and cervix. This gives the woman the opportunity to have a normal sex life and avoid the use of hormone replacement therapy. In addition, eggs stored in the ovaries can be used for surrogacy.
During the postoperative period of a hysterectomy, pain and bleeding always occur.
The pain bothers the woman for about a week and is nagging in nature. If the pain intensifies and becomes sharp and cramping, this indicates the development of complications.
Bloody discharge occurs due to the existence of a wound surface. By the end of the second week they gradually stop.
Long-term consequences are associated with a violation of the location of organs in the pelvis. The bladder moves backward, which can manifest itself in various urinary disorders. The intestines shift downward, which can ultimately cause prolapse of hemorrhoids.
If regional lymph nodes were removed along with the uterus, the outflow of lymph from the lower extremities is disrupted, which leads to the development of lymphostasis. This is manifested by swelling, heaviness, pain, and tissue malnutrition.
Conclusion
The organs of the female reproductive system are very complex. Knowledge of the anatomical structure of the reproductive system is necessary to understand the nature of pathological processes and diagnose diseases of the internal genital organs.
Read also...
- Why do you dream about a man’s back?
- Fortune telling with hearts online: a simple and free way to tell fortunes about a guy’s love
- Dream Interpretation: flying above the ground in a dream
- Description of orange zest with photo, its calorie content; how to make it at home; use of the product in cooking; harm and beneficial properties