Erythropoietin instructions for use in sports. Recombinant erythropoietin. Recombinant human erythropoietin. Erythropoietin test
recombinant human erythropoietin erythropoietinrecombinanthuman
Compound : in one bottle 1000/2000/5000 ME of epoetin-beta in the form of a lyophilized substance, which corresponds to 8.3/16.6/41.5 mcg of erythropoietin.
1 ampoule with solvent contains 1/2/5 ml of water for injection.
Epoetin-beta, obtained by genetic engineering, is identical in its amino acid composition, biological and immunological properties to erythropoietin isolated from the urine of patients suffering from anemia. Has the highest degree of purity. So far, there has been no evidence of the formation of antibodies to epoetin beta in humans.
Synonyms : Ergekh (Swr. "CilagA.G."), Recormon (Av. "BoehringerMannheim").
Pharmacological properties : Epoetin beta is a glycoprotein. Being a mitosis-stimulating factor and a cell differentiation hormone, it promotes the formation of red blood cells from precursor cells. Its production is carried out and regulated mainly in response to changes in tissue oxygenation. The therapeutic effect is manifested in an increase in the hematocrit number within 4 weeks. The course of treatment is 8-16 weeks (depending on dosage).
Pharmacokinetics : the half-life of epoetin-beta when administered intravenously is 4-12 hours. When administered subcutaneously, the maximum concentration of the drug in the serum is achieved on average after 12 hours, the final half-life is about 16 hours.
The bioavailability of epoetin beta when administered subcutaneously averages 46% of the bioavailability when administered intravenously.
Indications : erythropoietin replacement therapy for patients with renal anemia during dialysis.
Before starting treatment, other causes of anemia (deficiency of vitamin B12, folic acid, iron-aluminum intoxication) that reduce the effectiveness of erythropoietin should be excluded.
According to the literature, erythropoietin is effective for anemia in AIDS patients treated with zidovudine.
Contraindications : allergic reactions to any of the components of the erythropoietin drug, uncontrolled hypertension; the age of children under 2 years old, as well as the period of pregnancy and lactation (there is not enough experience).
Side effects : dose-dependent increase in blood pressure, exacerbation of existing hypertension (antihypertensive drugs should be prescribed, and blood pressure should be monitored between dialysis sessions and especially at the beginning of treatment). In some patients with normal and low blood pressure, a hypertensive crisis is possible with symptoms of encephalopathy (headaches, confusion, etc.) and generalized tonic-clonic seizures, requiring immediate medical attention and intensive care. Particular attention should be paid to sudden stabbing migraine-like headaches as a dangerous symptom.
Treatment with Recormon often requires an increase in the dose of heparin during dialysis due to an increase in hematocrit. In case of insufficient gelarinization, blockage of the dialysis system may occur.
Thrombosis of shunts is possible, especially in patients predisposed to hypotension, as well as with complications in the arteriovenous fistula (stenosis, aneurysm, etc.). In such patients, it is recommended to keep shunts under control and prevent thrombosis by prescribing acetylsalicylic acid.
It is also possible, especially at the beginning of treatment, to experience symptoms characteristic of the flu, headaches, a feeling of weakness, dizziness, bone pain, chills after the injection, convulsions, allergic reactions, fatigue.
Precautionary measures : erythropoietin should be prescribed with caution in cases of hypertension (including a history), malignant tumors, epilepsy (including a history), thrombocytosis, ischemic disease, sickle cell anemia, myocardial infarction, heart failure, arrhythmias, eczema, acne, febrile conditions, exanthema, osteomyelitis and necrosis of the feet, thrombosis of the inferior vena cava, exacerbation of occlusion of peripheral arteries, gastrointestinal and nasal bleeding, hematuria.
Erythropoietin can only be used in a hospital setting. After the first administration of the drug, the patient should be monitored, especially during the first four hours. Since an anaphylactoid reaction was reported during clinical trials, the first dose of erythropoietin should be administered under medical supervision. During treatment with the drug, weekly monitoring of blood pressure and blood counts, especially platelets, is necessary, which is especially important in the first 4 weeks (during treatment with the drug, there is a moderate, dose-dependent increase in the number of platelets within normal limits, especially after IV infusion, but as treatment continues it decreases; thrombocytosis develops very rarely). Periodic monitoring of the hematocrit number is also necessary until the value reaches 30-35 vol.% (hemoglobin 10-12 g/dL), then it should be monitored weekly. In most cases, with an increase in the hematocrit number, the content of ferritin in the serum simultaneously decreases. Therefore, when serum ferritin levels are below 100 ng/ml or transferrin saturation is less than 20%, oral iron is recommended at a dose of 200-300 mg/day, and, if necessary, parenterally. If iron supplements are prescribed, the dose of erythropoietin should be reduced to prevent an intense increase in hemoglobin.
During the correction of anemia, an increase in appetite is possible, which can lead to increased potassium consumption and hyperkalemia. During the first months of treatment with erythropoietin, serum potassium, creatinine, urea and phosphate levels should be monitored. Sometimes an increased dose of phosphate binders (eg calcium carbonate) is required. It is necessary to monitor liver function and metabolism. In patients with aluminum toxicity or infections, the effect of erythropoietin may be delayed or weakened. In patients receiving anticonvulsant therapy, seizures may increase.
In some cases, the drug may cause a transient increase in predialysis levels of urea, creatinine and potassium, which can be explained by a decrease in plasma flow or an increase in protein intake. Typically, these indicators decrease after correction of blood flow. No significant changes in dialysis regimen were observed with erythropoietin treatment.
In patients with a kidney transplant in combination with sickle cell anemia, epoetin beta can cause acute hemolysis with graft rejection.
The treatment may affect the body's reactivity (the ability to perform work that requires quick physical and mental reactions), especially at the beginning of treatment and when drinking alcohol.
Drug interactions : when treating with erythropoietin with the simultaneous use of antihypertensive drugs, individual dose selection is possible.
The therapeutic activity of erythropoietin can be enhanced by the simultaneous administration of drugs that affect hematopoiesis (iron preparations, etc.).
No interaction of erythropoietin with other substances was detected during clinical trials.
Application and dosage : the contents of the vial are dissolved in the supplied solvent, ensuring that the concentration of epoetin beta does not exceed 2000 IU/ml. The resulting solution should be light and transparent. It is administered subcutaneously or intravenously. Unused remains of the solution in the vial must be destroyed. The solution is injected into the vein slowly (about 2 minutes). For patients undergoing hemodialysis, the solution is administered through an arteriovenous fistula after dialysis. The biological activity of the prolonged solution remains unchanged for 24 hours at a temperature of 2 to 8°C. However, to ensure sterility, the prepared solution should be used immediately. To avoid incompatibility or decrease in the activity of the drug, it is not recommended to: use another solvent, mix the drug with other drugs or injection solutions, use glass (use only plastic materials for injection).
Treatment with erythropoietin is carried out in two stages.
AT THE CORRECTION STAGE, the hematocrit number should increase from 30 vol.% to 35 vol.%. For subcutaneous administration, the initial dose is 20 IU/kg body weight 3 times a week or 10 IU/kg 7 times a week. If the hematocrit increase is insufficient (less than 0.5 vol.% per week), the dose can be increased every 4 weeks by 20 IU/kg 3 times a week or by 10 IU/kg 7 times a week. When administered intravenously, the initial dose is 40 IU/kg 3 times a week. After 4 weeks, the dose can be increased to 80 IU/kg 3 times a week. If necessary, it is increased by 20 IU/kg 3 times a week at monthly intervals.
Regardless of route of administration, the maximum dose should not exceed 720 IU/kg per week.
If the hematocrit number increases too quickly, i.e. more than 4% within 2 weeks, the dose of the drug should be reduced by approximately 20 IU/kg.
AT THE STAGE OF MAINTAINING the hematocrit at 30-35 vol.%, the initial maintenance dose should be reduced to half the dose of the previous injection. Then the maintenance dose is selected individually in one or two weeks so that the hematocrit number does not exceed 35 vol.%.
The average maintenance dose is approximately 30 IU/kg 3 times a week after hemodialysis.
Overdose : individual and dose-dependent. In case of overdose, hypertension and erythrocytosis may develop. If you have hypertension, fluid loading should be avoided. In case of erythrocytosis and hyperhydration, before losing weight by removing fluid from the body, it is necessary to perform a venesection. Otherwise, a further increase in the hematocrit number may occur, which entails an increase in viscosity. In case of resistant hypertension, the prescription of antihypertensive drugs is indicated.
Form releasing : the package contains 5/10 vials with lyophilized substance and 5/10 ampoules with solvent.
Storage : at a temperature of 2-8°C (in the refrigerator). During transportation, changes in temperature conditions are allowed, but no more than 5 days.
Recormon should not be used after the expiration date stated on the packaging.
Dosage form: solution for intravenous and subcutaneous administration Compound:1 ml of solution contains:
Active substance:
Recombinant human erythropoietin 500
ME or 2000ME.Excipients:
Albumin solution 10% (in terms of dry albumin) - 2.5 mg.
Isotonic citrate buffer: sodium citrate -5.8 mg, sodium chloride -5.84 mg, citric acid - 0.057 mg, water for injection - up to 1 ml.
Description:Transparent colorless liquid
Pharmacotherapeutic group:hematopoiesis stimulator ATX:B.03.X.A Other hematopoiesis stimulants
Pharmacodynamics:Epoetin beta is a glycoprotein that specifically stimulates erythropoiesis, activates mitosis and maturation of erythrocytes from erythrocyte precursor cells. Recombinant is synthesized in mammalian cells into which the gene encoding human erythropoietin is embedded. According to its composition, biological
and immunological properties are identical to natural human erythropoietin. The administration of epoetin beta leads to an increase in hemoglobin and hematocrit, improving blood supply to tissues and heart function. The most pronounced effect of the use of epoetin beta is observed in anemia caused by chronic renal failure. In very rare cases, with long-term use of erythropoietin for the treatment of anemic conditions, the formation of neutralizing antibodies to epoetin beta may be observed with or without the development of partial red cell aplasia. Pharmacokinetics:With intravenous administration of Erythropoietin in healthy individuals and patients with uremia, the half-life is 5-6 hours. With subcutaneous administration of Erythropoietin, its concentration in the blood increases slowly and reaches a maximum in the period from 12 to 28 hours after administration, the half-life is 13-28 hours. When administered intravenously, the half-life is 4-12 hours. The bioavailability of Erythropoietin when administered subcutaneously is 25-40%.
Indications:Treatment of anemia of renal origin in patients with chronic renal failure, incl. on dialysis.
Prevention and treatment of anemia in adult patients with solid tumors receiving chemotherapy with platinum drugs, which can cause anemia (75 mg/m2 per cycle, 350 mg/m2 per cycle).
Treatment of anemia in adult patients with multiple myeloma, low-grade non-Hodgkin's lymphoma and chronic lymphocytic leukemia receiving antitumor therapy with a relative deficiency of endogenous erythropoietin (defined as a serum erythropoietin concentration that is disproportionately low relative to the degree of anemia).
Increasing the volume of donor blood intended for subsequent autotransfusion. At the same time, the benefits of using epoetin beta must be weighed against the increased risk of thromboembolism with its use. For patients with moderate anemia (hemoglobin level 100-130 g/l or hematocrit 30-39%, without iron deficiency), the drug is prescribed only if it is not possible to obtain a sufficient amount of canned blood, and planned major surgery may require a large volume blood (>4 units for women or >5 units for men).
Prevention of anemia in premature newborns born with a body weight of 750-1500 g, up to 34 weeks of pregnancy.
Contraindications:Hypersensitivity to the drug or its components, partial red cell aplasia after previous therapy with any epoetin beta, uncontrolled hypertension, failure to receive adequate anticoagulant therapy, myocardial infarction within a month after the event, unstable angina, or increased risk of deep vein thrombosis and thromboembolism in as part of a pre-deposit blood collection program before surgery, porphyria.
Carefully:in patients with thrombosis (history), with malignant neoplasms, with sickle cell anemia, with moderate anemia without iron deficiency, with thrombocytosis, with refractory anemia, epilepsy, chronic liver failure, nephrosclerosis, in patients with body weight less than 50 kg to increase volume donated blood for subsequent autotransfusion Pregnancy and lactation:Since humans do not have sufficient experience with the use of erythropoietin during pregnancy and breastfeeding, Erythropoietin should be prescribed only if the expected benefits from its use outweigh the possible risk to the fetus and mother.
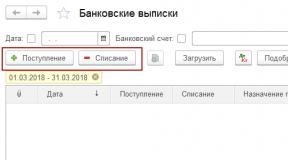
Directions for use and dosage:Treatment of anemia in patients with chronic renal failure,
P/c or i.v. When administered intravenously, the solution should be administered within 2 minutes; for patients on hemodialysis - through an arteriovenous shunt at the end of the dialysis session. For patients not on hemodialysis, it is preferable to administer the drug subcutaneously to avoid puncture of peripheral veins.
The goal of treatment is to achieve a hematocrit level of 30-35% or eliminate the need for blood transfusion. The weekly increase in hematocrit should not exceed 0.5%. Its level should not exceed 35%. In patients with arterial hypertension, cardiovascular and cerebrovascular diseases, the weekly increase in hematocrit and its target values should be determined individually, depending on the clinical picture. For some patients, the optimal hematocrit is below 30 %.
Treatment with Erythropoietin is carried out in 2 stages:
Initial therapy (correction stage).
For subcutaneous administration, the initial dose is 20 IU/kg body weight 3 times a week. If the increase in hematocrit is insufficient (less than 0.5% per week), the dose can be increased monthly by 20 IU/kg body weight 3 times a week. The total weekly dose can also be divided into daily administrations in smaller doses or administered in one go.When administered intravenously, the initial dose is 40 IU/kg body weight 3 times a week. If the hematocrit does not increase sufficiently after a month, the dose can be increased to 80 IU/kg 3 times a week. If there is a need to further increase the dose, it should be increased by 20 IU/kg 3 times a week at monthly intervals. Regardless of the route of administration, the highest dose is no more than 720 IU/kg body weight per week.
Maintenance therapy.
To maintain the hematocrit at 30-35%, the dose should first be reduced by half from the dose in the previous injection. Subsequently, the maintenance dose is selected individually, with an interval of 1-2 weeks. With subcutaneous administration, the weekly dose can be administered once or in 3-7 injections per week.
In children, the dose depends on age (as a rule, the younger the child, the higher doses of epoetin beta he needs). However, since it is not possible to predict individual response, it is advisable to start with the recommended regimen.
Treatment with Erythropoietin is usually lifelong. If necessary, it can be interrupted at any time.
Prevention of anemia in premature newborns.
SC at a dose of 250 IU/kg body weight 3 times a week. Treatment with epoetin beta should begin as early as possible, preferably from the 3rd day of life, and continue for 6 weeks.
Prevention and treatment of anemia in patients with solid tumors.
SC, dividing the weekly dose into 3-7 injections.
For patients with solid tumors receiving platinum chemotherapy, treatment with Erythropoietin is indicated if the hemoglobin level before chemotherapy is not higher than 130 g/l. The initial dose is 450 IU/kg body weight per week. If after 4 weeks the hemoglobin level does not increase sufficiently, the dose should be doubled. The duration of treatment is no more than 3 weeks after the end of chemotherapy.
If during the first cycle of chemotherapy, the hemoglobin level, despite treatment with epoetin beta, decreases by more than 10 g/l, further use of the drug may not be effective.
An increase in hemoglobin by more than 20 g/l per month or to a level above 140 g/l should be avoided. If hemoglobin increases by more than 20 g/l per month, the dose of epoetin beta should be reduced by 50%. If the hemoglobin level exceeds 140 g/l, the drug is discontinued until it drops to the level<120 г/л, а затем возобновляют терапию в дозе, наполовину меньшей предшествующей недельной.
Treatment of anemia in patients with myeloma , low-grade non-Hodgkin's lymphoma or chronic lymphocytic leukemia.
Patients with multiple myeloma, low-grade non-Hodgkin's lymphoma, or chronic lymphocytic leukemia usually have a deficiency of endogenous erythropoietin. It is diagnosed by the relationship between the degree of anemia and the insufficient concentration of erythropoietin in the serum.
Relative deficiency of erythropoietin occurs:
| At hemoglobin level, g/l | Serum erythropoietin concentration, IU/ml |
| > 90 <100 | < 100 |
| > 80 < 90 | <180 |
| <80 | <300 |
The above parameters should be determined no earlier than 7 days after the last blood transfusion and the last cycle of cytotoxic chemotherapy.
The drug is administered subcutaneously; The weekly dose can be divided into 3 or 7 injections. The recommended starting dose is 450 IU/kg body weight per week. If after 4 weeks the hemoglobin level increases by at least 10 g/l, treatment is continued at the same dose. If after 4 weeks hemoglobin increases by less than 10 g/l, the dose can be increased to 900 IU/kg body weight per week. If after 8 weeks of treatment the hemoglobin level has not increased by at least 10 r/l, a positive effect is unlikely and the drug should be discontinued.
Clinical studies have shown that in chronic lymphocytic leukemia, the response to epoetin beta therapy occurs 2 weeks later than in patients with multiple myeloma, non-Hodgkin's lymphoma and solid tumors. Treatment should be continued until 4 weeks after the end of chemotherapy.
The highest dose should not exceed 900 IU/kg body weight per week.
If within 4 weeks of treatment the hemoglobin level increases by more than 20 g/l, the dose of Erythropoietin should be reduced by half. If the hemoglobin level exceeds 140 g/l, treatment with the drug should be interrupted until it decreases to the value<130 г/л, после чего терапию возобновляют в дозе, наполовину меньшей предшествующей недельной. Лечение следует возобновлять только в том случае, если наиболее вероятной причиной анемии является недостаточность Эритропоэтина.
Preparing patients for the collection of donor blood for subsequent autohemotransfusion.
IV or SC twice a week for 4 weeks. In cases where the patient’s hematocrit (>33%) allows blood sampling, it is administered at the end of the procedure. Throughout the course of treatment, the hematocrit should not exceed 48%.
The dose of the drug is determined by the transfusiologist and the surgeon individually, depending on the volume of blood that will be taken from the patient and his erythrocyte reserve. The volume of blood that will be taken from the patient depends on the estimated blood loss, available blood conservation techniques and the general condition of the patient; it must be sufficient to avoid a blood transfusion from another donor. The volume of blood that will be taken from the patient is expressed in units (one unit is equivalent to 180 ml of red blood cells).
The possibility of donation depends mainly on the blood volume of a given patient and the initial hematocrit. Both indicators determine the endogenous erythrocyte reserve, which can be calculated using the following formula:
endogenous erythrocyte reserve= blood volume (ml) x (hematocrit - 33): 100
women: blood volume (ml) = 41 (ml/kg) x body weight (kg) + 1200 (ml)
men: blood volume (ml) = 44 (ml/kg) x body weight (kg) + 1600 (ml) (for body weight >45 kg).
Indications for the use of Erythropoietin and its single dose are determined by nomograms, based on the required volume of donor blood and endogenous erythrocyte reserve.
The highest dose - with intravenous administration is no more than 1600 IU/kg body weight per week; with subcutaneous administration - 1200 IU/kg body weight per week.
Side effects:Adverse reactions are listed according to the following gradation: often (>1%,<10%); нечасто (>0,1 %, <1 %); редко (>0,01 %, <0,1 %); очень редко (<0,01 %), включая отдельные сообщения.
From the cardiovascular system:
in patients with anemia with chronic renal failure, the most common is an increase in blood pressure (BP) or an increase in existing arterial hypertension, especially in the case of a rapid increase in hematocrit. In this case, it is recommended to prescribe drug antihypertensive therapy; if there is no effect, it is recommended to temporarily interrupt therapy with epoetin beta. In some patients (including those with previously normal or low blood pressure) - a hypertensive crisis with symptoms of encephalopathy (headaches, confusion, sensory and motor disorders - speech disorders, gait, up to tonic-clonic convulsions), requiring emergency medical attention care and intensive care. Particular attention should be paid to sudden migraine-like pain.Patients with solid tumors, multiple myeloma, non-Hodgkin's lymphoma or chronic lymphocytic leukemia may rarely experience headaches and increased blood pressure, which can be relieved by the administration of drugs.
From the hematopoietic organs: in patients with renal failure and anemia, a dose-dependent increase in the number of platelets (not beyond the normal range and disappearing with continued therapy) may occur, especially after intravenous administration. Thrombocytosis develops very rarely. Due to increased hematocrit, it is often necessary to increase the dose of heparin during hemodialysis. Inadequate heparinization may result in blockage of the dialysis system. Shunt thrombosis may develop, especially in patients with a tendency to hypotension or with complications of an arteriovenous fistula (for example, stenosis, aneurysm, etc.). In such situations, early revision of the shunt and timely prevention of thrombosis (acetylsalicylic acid) are recommended.
In most cases, along with an increase in hematocrit, the serum ferritin level decreases. In some cases, in patients with uremia - increased levels of potassium and phosphate in the serum.
Some patients with solid tumors, myeloma, non-Hodgkin's lymphoma, or chronic lymphocytic leukemia have decreased serum iron metabolism. Clinical studies have shown that the incidence of thromboembolism in cancer patients treated with Erythropoietin is slightly higher than in the absence of such therapy or when using placebo; however, a clear causal relationship with the drug has not been established.
In premature newborns, in most cases there is a decrease in serum ferritin, and there may be a slight increase in the number of platelets, especially at 12-14 days of life.
In patients preparing to donate blood for subsequent autotransfusion and receiving, there is an increase in the number of platelets, usually not beyond normal limits, and a higher incidence of thromboembolic complications, although their causal relationship with the use of the drug has not been established.
Other: rarely - allergic skin reactions in the form of rash, itching, urticaria or reactions at the injection site. Isolated cases of anaphylactoid reactions have been described. However, in controlled clinical studies, the incidence of hypersensitivity reactions did not increase.
In some cases, especially at the beginning of therapy, flu-like symptoms such as fever, chills, headache, pain in the limbs and bones, and malaise were noted.
These reactions were mild or moderate and disappeared within a few hours or days.
Overdose:Symptoms: hypertension, erythrocytosis, hyperhemoglobinemia, sharp increase
hematocrit values.
Treatment: symptomatic. In case of hypertension, it is necessary to avoid excessive hydration. In the presence of erythrocytosis and hyperhydration, measures to remove excess fluid are necessary.
If hemoglobin and hematocrit levels are high, phlebotomy is indicated.
Interaction: With the simultaneous use of Erythropoietin and cyclosporine, it may be necessary to adjust the dose of the latter due to an increase in its binding to erythrocytes. Experience in the clinical use of Erythropoietin to date has not revealed evidence of its pharmacological incompatibility with other drugs. However, to avoid possible incompatibility or reduced activity. Erythropoietin should not be mixed with solutions of other drugs. Special instructions:Since anaphylactoid reactions have been reported in some cases, the first dose of the drug should be administered under the supervision of a physician.
Inappropriate use of the drug by healthy people (for example, as doping) can cause a sharp increase in hematocrit, accompanied by life-threatening complications from the cardiovascular system.
During treatment, it is necessary to monitor blood pressure weekly and perform a complete blood count, including determination of hematocrit, platelets and ferritin. In the first 8 weeks of therapy, weekly counts of formed elements and especially platelets are necessary. If the platelet count increases above normal or by more than 150 109/l from the initial value, treatment with Erythropoietin should be interrupted.
In patients with uremia undergoing hemodialysis, it is recommended to monitor blood pressure, incl. between dialysis sessions. Due to an increase in hematocrit, it is often necessary to increase the dose of heparin; in addition, timely prevention of thrombosis and early revision of the shunt are necessary. In the pre- and postoperative period, hemoglobin should be monitored more often if its initial level was less than 140 g/l. During treatment with Erythropoietin, it is necessary to periodically monitor the level of potassium and phosphate in the blood serum. If hyperkalemia occurs, Erythropoietin should be temporarily discontinued until potassium concentrations normalize.
In most cases, along with an increase in hematocrit, serum ferritin levels decrease. Therefore, all patients with anemia of renal origin and with a serum ferritin level of less than 100 mcg/l or transferrin saturation of less than 20% are recommended to take oral iron supplements at a dose of 200-300 mg/day. Patients with oncological and hematological diseases are treated with iron supplements according to the same principles, while patients with multiple myeloma, low-grade non-Hodgkin's lymphoma or chronic lymphocytic leukemia with transferrin saturation less than 25% can be given 100 mg of iron per week IV.
For premature infants, oral iron therapy at a dose of 2 mg per day should be prescribed as early as possible (no later than the 14th day of life). The dose of iron is adjusted depending on the level of serum ferritin. If it persistently remains at a level below 100 mcg/ml or there are other signs of iron deficiency, the dose of iron supplements should be increased to 5-10 mg/day and therapy should be continued until the signs of iron deficiency are relieved.
When using Erythropoietin in women of reproductive age, menstruation may resume. The patient should be warned about the possibility of pregnancy and the need to use reliable methods of contraception before starting therapy.
Given the possible more pronounced effect of Erythropoietin, its dose should not exceed the dose of epoetin beta used in the previous course of treatment. During the first two weeks, the dose is not changed and the dose/response ratio is assessed. After this, the dose can be reduced or increased according to the scheme presented above.
During the treatment period, until the optimal maintenance dose is established, patients with uremia should avoid engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions, due to an increased risk of increased blood pressure at the beginning of therapy.
Release form/dosage:Solution for intravenous and subcutaneous administration 500 IU/ml or 2000 IU/ml Package:In ampoules of 1 ml. 5 ampoules in a blister pack, 1 or 2 blister packs and instructions for use in a cardboard pack.
Storage conditions:In a dry place, protected from light, at a temperature of 2 to 8 °C.
Keep out of the reach of children!
Best before date:2 years. Do not use after the expiration date.
Conditions for dispensing from pharmacies: On prescription Registration number: LS-001854 Registration date: 19.12.2011 Owner of the Registration Certificate: BINNOPHARM, CJSC Russia Manufacturer: Information update date: 15.11.2015 Illustrated instructionsLatin name: Erythropoietin
ATX code: B03XA01
Active substance: epoetin beta
Manufacturer: Binnopharm, Russia
Dispensing from the pharmacy: On prescription
Storage conditions: darkness, dryness
Best before date: two years.
Erythropoietin is a lyophilisate from which a solution is prepared for intramuscular or intravenous administration. A product based on epoetin beta is a recombinant renal hormone that increases the number of reticulocytes and red blood cells in the blood and promotes the formation of hemoglobin in cells.
Erythropoietin is used for all kinds of anemia. If the drug is intolerated or used incorrectly, a heart attack or stroke may develop. Therefore, the drug is dispensed only for medical prescription.
Composition and release form
Erythropoietin is produced in the form of a dry concentrate, from which a solution is prepared for intramuscular or intravenous administration. 1 ml of medicinal liquid contains epoetin beta in the amount of 2000 IU or 500 IU.
Supporting cast:
- Isotonic citrate – E 330
- Sodium chloridum
- E 331
- Albumin protein solution.
The colorless solution is placed in ampoules (1 ml each). A pack of thick paper can contain 5 or 10 ampoules.
Another form of release of the drug is Erythropoietin alpha. The solution contains 20,000 or 10,000 IU of epoetin.
Additional components:
- E 433
- Injection water
- Sodium hydrogen phosphate
- Sodium chloride.
The colorless solution is packaged in ampoules (10,000 units), vials (10,000 units, 4,000 units, 2,000 units), syringes (1,000 units - 4,000 units).
Pharmacological properties
Epoitin beta is a glycoprotein that activates mitosis, erythropoiesis and promotes the formation of red blood cells. Recombinant Erythropoietin is produced in vertebrate cells, where a gene is introduced that blocks human epoitin.
Epoetin beta is similar to erythropoietin produced in the human body. After using the solution, hematocrit and hemoglobin levels increase.
If you use epoetin beta in the treatment of young women, their menstrual cycle will improve. But the risk of pregnancy also increases, so contraception must be used during treatment.
The use of Erythropoietin stimulates blood circulation in tissues and improves cardiac activity. The administration of Epoetin is effective for anemia that occurs against the background of renal failure. However, with prolonged use of the drug, neutralizing antibodies to its components may form, followed by the occurrence of erythroblastopenia.
When using the solution intramuscularly, the half-life takes up to 6 hours. With long-term use of the product, the content of its basic components in plasma becomes maximum 12-28 hours after use. T ½ - from 13 to 28 hours.
With intravenous administration, T1/2 takes 4-12 hours. When used intramuscularly, bioavailability is 25-40%.
Indications and contraindications for use
Erythropoietin is used for preventive and therapeutic purposes for anemia of various etiologies, including hematological syndrome in chronic renal failure and iron deficiency anemia in patients on hemodialysis.
The remedy is also used for anemia accompanied by the following conditions:
- Myeloma
- Presence of large tumors treated with chemotherapy
- Lymphocytic leukemia
- Erythropoietin deficiency.
Erythropoietin is prescribed to increase the amount of donor blood for blood transfusion. The solution is also used to prevent anemia in premature babies.
- Contraindications:
- Epoetin intolerance
- Heart attack
- Pregnancy
- Severe vascular pathologies
- Stroke
- Erythroblastopenia occurring after taking epoetin
- Porphyria
- Thrombosis
- Hypertension
- Lactation.
Treatment will be ineffective for iron deficiency, acute inflammatory or infectious process and hemolysis, in which hemoglobin is released.
Instructions for use

The cost of the medicine is from 7,300 rubles. The price of the medicine is from 4422 rubles.
The instructions for use state that Erythropoietin is used intravenously or subcutaneously. Intravenous administration of the medication should last about two minutes. In hemodialysis, the drug is used at the final stage of the procedure and is administered through an arteriovenous shunt.
For chronic renal failure and anemia in adults, Erythropoietin is administered subcutaneously three times a week. Dosage – 20 IU/kg. If the hematocrit is less than 0.5%, then the amount of the drug increases by 20 IU/kg every 30 days. The maximum dose is 720 IU/kg.
During maintenance treatment, the initial amount of Erythropoietin with a hematocrit of 30% is achieved by administering a dosage of ½ of the previous injection. Then the dose is selected for each patient individually. Dosage adjustments are made every 7-14 days.
For anemia in children, the dose is selected based on the child’s age. The duration of therapy is lifelong. You can interrupt treatment at any time.
Erythropoietin dosage:
- Anemia in premature babies - 250 IU/kg IM three times a week. The medicine begins to be used on the 3rd day after birth. Therapy lasts one and a half months.
- Anemia due to tumor formations – 450 IU/kg once a week. If treatment is ineffective, the dose may be doubled. Treatment time is up to 21 days.
- Anemia in myeloma, leukemia, lymphoma - subcutaneously 450 IU/kg every 7 days or 3-7 times a week. If necessary, the dose can be increased to 900 IU/1 kg.
In preparation for transfusion of one's own blood, Erythropoietin is administered by any method twice a week for one month. When the hematocrit is more than 33%, the solution can be administered at the final stage of the procedure.
The highest dose per week for intravenous administration is 1600 IU/1 kg of body weight. The maximum amount for intramuscular use is 1200 IU/1 kg.
Erythropoietin is often used in bodybuilding for better tissue nutrition. The amount varies from 50 to 300 units/kg. Erythropoietin can be used continuously in sports for no more than 1.5 months.
Side effects, overdose, interactions
Due to intramuscular or intravenous administration of the drug, erythropoietins can provoke a number of negative reactions. These are hyperkalemia, encephalopathy, thrombocytosis, migraine, anaphylaxis.
Other side effects:
- Skin rashes
- Chills
- Brain fog
- Hypertension
- Convulsions
- Fever
- Ossalgia
- Dislalia.
Overdose is manifested by a sudden increase in hematocrit and hemoglobin in the blood, hypertension, erythrocytosis. Treatment involves using phlebotomy and removing excess fluid from the body.
Interaction of Erythropoietin with other drugs:
- Medicinal solutions – may reduce the effectiveness of epoetin
- Cyclosporine - increases the binding of red blood cells, which requires dose adjustment.
Analogs
 Manufacturer – Roche Diagnostics, Germany
Manufacturer – Roche Diagnostics, Germany
Price– from 1060 rubles
Description – the solution is used for the treatment and prevention of anemia
pros– can be transported without refrigeration, efficiency
Minuses– price, many side effects, after administration, local negative reactions often occur in the form of itching, redness and swelling, which can provoke a stroke or heart attack.
 Manufacturer – Pharmapark, Russia
Manufacturer – Pharmapark, Russia
Price– 3800 rubles
Description – the solution is used for anemia that occurs in premature babies, for malignant tumors, multiple myeloma, leukemia, erythropoietin deficiency
pros– quickly eliminates signs of anemia, increases blood supply to tissues
Minuses– cost, ampoules are inconvenient to open, cannot be used for diseases of the heart and blood vessels.
Erythropoietin (EPO) is a glycoprotein hormone that controls the rate of erythropoiesis in the human body. The substance presented is synthesized mainly in the kidneys, a small amount (about 10 percent) is formed in the liver. The hormone erythropoietin activates the division and differentiation of erythroid precursors. The level of endogenous hormone in the blood plasma of healthy people varies over a wide range and is inversely related to the concentration of hemoglobin and the degree of tissue oxygenation. The work on isolating and producing this hormone for medical purposes is very useful.
Structure and significance of the hormone
The hormone molecule consists of amino acids. With a deficiency of endogenous erythropoietin, a sharp decrease in the level of hemoglobin and red blood cells in the blood is observed, and the so-called erythropoietin deficiency anemia develops. Until recently, drug correction of such anemia remained impossible due to the lack of appropriate pharmaceuticals. Nowadays, when there is a deficiency of the above hormone in the human body, doctors prescribe recombinant erythropoietin. The drug is obtained from animal cells into which the gene code for human EPO is introduced. Recombinant human erythropoietin is identical in amino acid and carbohydrate composition to the natural hormone, increases the number of red blood cells, reticulocytes, and activates hemoglobin biosynthesis in cells. The biological activity of the resulting substance is no different from the endogenous hormone. Recombinant erythropoietin does not exhibit cytotoxic effects and does not affect leukopoiesis. Scientists suggest that EPO interacts with specific erythropoietin-sensitive receptors that are localized on the cell surface.

Method for purifying recombinant human erythropoietin
Recombinant human EPO is one of the most common proteins produced by many biological and pharmaceutical companies around the world for drug therapy. The presented compound is synthesized by Chinese hamster ovary (CHO) cells using the recombinant DNA method. One polypeptide chain of recombinant EPO contains 165 amino acids, the calculated molecular weight of which is 24,000 Da, and the observed molecular weight of the glycosylated protein is 30,400 Da. Separation of erythropoietin from impurities is carried out using ion exchange and Human recombinant EPO has a purity of 98%.
Recombinant erythropoietins and their analogues
To stimulate the processes of erythropoiesis, doctors use different drugs:
- "Aranesp";
- "Aeprin";
- "Epobiocrine";
- "Bioein";
- "Vepox";
- "Binocrit";
- "Epocrine";
- "Gemaks";
- "Epogen";
- "Eprex";
- "Epovitan";
- "Epomax";
- "Hypercrit";
- "Eralfon";
- "Erytrostim";
- "Recormon";
- "Epostim";
- "Eposino";
- Epoetin Beta.
Before replacing recombinant erythropoietin with analogs, you should consult with your doctor.

Indications for use
Medical practitioners quite often have to deal with erythropoietin deficiency anemia (EDA). This group includes the following pathologies:
- anemia in malignant neoplasms;
- early anemia of premature babies (up to 34 weeks of pregnancy) with body weight from 750 to 1500 g;
- nephrogenic anemia;
- anemia in chronic diseases (hepatitis C, rheumatoid arthritis, HIV infection, diseases of the digestive canal).
A distinctive feature of the above anemias is that they are not treated with iron supplements. Until recently, the only effective treatment method was blood transfusions. Due to the fact that this type of therapy has a huge number of side effects and a high risk of transmitting pathogens of a number of dangerous infectious diseases (HIV, hepatitis viruses, etc.) through the blood, this method is practically not used in modern medicine. Recombinant human erythropoietin helps improve the quality of life of patients diagnosed with erythropoietin deficiency anemia. The biosynthesis and introduction into practice of recombinant human EPO has opened a new era in the treatment of erythropoietin-dependent anemia.

Contraindications
- thromboembolism;
- hypersensitivity to the drug;
- inability to carry out effective anticoagulant therapy;
- previous cerebral stroke or myocardial infarction;
- unstable angina;
- uncontrolled arterial hypertension;
- the period of bearing a child and breastfeeding;
- refractory arterial hypertension.

Dosage regimen
The dosage, regimen and duration of treatment are established on a strictly individual basis, depending on the severity of anemia, the general condition of the patient and the nature of the pathology. The drugs are intended for parenteral use. Initial doses range from 50 to 150 IU/kg. The dose must be adjusted depending on the patient's age. Recombinant erythropoietin is usually administered 3 times a week. With an overdose of the drug, increased side effects are observed. The result becomes more or less noticeable after 2-3 weeks of use.
Side effect
Are you prescribed recombinant human erythropoietin? Instructions for use do not exclude the development of side effects. This:
- myalgia;
- dizziness;
- hyperthermia;
- drowsiness;
- vomit;
- headache;
- diarrhea;
- arthralgia;
- hypertension;
- chest pain;
- thrombocytosis;
- tachycardia;
- hypertensive crisis;
- convulsions;
- hepatosis;
- increased activity levels of AST, ALT in the blood;
- erythrocyte lineage aplasia;
- eczema;
- angioedema;
- skin rash and itching;
- asthenia;
- urticaria, hyperemia and burning at the injection site;
- hyperkalemia;
- decreased concentration of ferritin protein in blood plasma;
- hyperphosphatemia.

Erythropoiesis stimulants in sports
Recently, the drug Epovitan (recombinant human erythropoietin) is often used. The presented product is often used in sports (athletics, bodybuilding, swimming, biathlon). This drug activates the biosynthesis of red blood cells, which, in turn, leads to an increase in the oxygen content per unit volume of blood and, accordingly, to an increase in the oxygen capacity of the blood and the delivery of O 2 to organs and tissues. This mechanism of action increases the athlete’s aerobic endurance. A similar effect is observed when an athlete trains in mid-altitude conditions, when a lack of O 2 in the air provokes the development of hypoxia, which, in turn, activates the biosynthesis of endogenous erythropoietin. EPO preparations are used in combination with insulin, somatotropin (GH, growth hormone) and stanazolol.
Excessive, uncontrolled use of the drug "Erythropoietin" in sports can provoke the formation of blood clots, which is usually fatal. It is quite difficult to detect recombinant EPO, since the structure of the synthetic compound is identical to its physiological counterpart, therefore this biocompound is still used illegally in professional sports as a doping.
The hormone erythropoietin regulates the formation of electrocytes (red blood cells), which are synthesized in stem cells of the bone marrow. This biologically active substance is produced by the kidneys and, to a much lesser extent, by the liver, and its production is influenced by the concentration of oxygen in the blood: when its level begins to decrease, the amount of erythropoietin increases and stops increasing as soon as the body is saturated with oxygen.
Erythroepin is considered a physiological stimulator of erythropoiesis (this is what one of the processes of hematopoiesis is called). Its production begins as soon as oxygen begins to flow into the body’s tissues in excessively small quantities (it is transported mainly by the complex iron-containing protein hemoglobin).
It is worth noting that the role of oxygen is extremely important, since it is with its participation that the energy necessary for the life of the body is produced. It takes part in oxidative processes, as well as in various metabolic reactions, including the synthesis of cholesterol, bile acids, steroid hormones, and biologically active products of amino acid metabolism. Also, its presence is necessary to neutralize poisons, toxins, and drugs.
If the amount of oxygen in the blood decreases and is not restored, hypoxia occurs, which leads to disturbances in the biochemical processes of tissue respiration. The muscles of the heart, central nervous system, kidneys and liver are especially affected.
To prevent irreversible consequences, the kidneys, in response to oxygen starvation or ischemia (circulatory disturbance), produce erythropoiesis to stimulate erythropoiesis. The hormone, entering the blood, activates the transformation of reticulocytes into red blood cells. As a result, hematopoiesis increases, and more red blood cells are released into the blood.
As a result, the level of oxygen in the blood increases, which leads to improved cell nutrition and, accordingly, makes the body more resilient. In addition, under the influence of erythropoietin, systemic blood pressure increases, and due to an increase in erythrocyte mass, blood viscosity increases.
Also, the kidneys increase the production of the hormone in case of blood loss, any form of anemia, or insufficient blood supply to the kidneys. The concentration of erythropin in the blood may increase under the influence of glucocorticoids. This is the name of the hormones produced by the adrenal cortex, the production of which increases during stressful situations. An increase in erythropoietin in this case leads to an increase in the amount of hemoglobin and the oxygen-supplying capacity of the blood during stress.
 Another effect of the hormone on the blood is that under its influence the bone marrow increases the intake of iron, copper, vitamins B9, B12. This leads to a decrease in these elements in the blood plasma, as well as a decrease in transport proteins: feritin, which is responsible for storing iron in the body, and transcobalamin (B12). Therefore, you need to take care of your diet and ensure that your body receives the right amount of vitamins and minerals every day.
Another effect of the hormone on the blood is that under its influence the bone marrow increases the intake of iron, copper, vitamins B9, B12. This leads to a decrease in these elements in the blood plasma, as well as a decrease in transport proteins: feritin, which is responsible for storing iron in the body, and transcobalamin (B12). Therefore, you need to take care of your diet and ensure that your body receives the right amount of vitamins and minerals every day.
Above and below normal
The concentration of erythropoietin in the blood of a healthy woman ranges from 8 to 30 IU/l; in men, these figures range from 5.6 to 28.9 IU/l. Deviations from the norm make the doctor wary and prescribe additional examination to determine the cause.
For example, if the level of erythropoietin is increased and the number of red blood cells is decreased (this despite the fact that the hormone promotes their production), this indicates the development of anemia (anemia), which provoked suppression of bone marrow function. If, during anemia, tests show a reduced amount of the hormone, this indicates that the kidneys synthesize its production less than normal.
In addition to comparing these tests, hormones and the environment influence the increase or decrease of erythropoietin. For example, a high concentration of estrogen in the blood reduces the production of erythropoietin, while thyroid hormones, somatropin, testosterone, prostaglandins, and glucocorticoids increase it. Erythropoietin also increases due to smoking, low partial air pressure, and exposure to high altitudes.
A reduced amount of erythropoietin indicates kidney problems, primarily chronic renal failure (which is why people with this disease suffer from anemia). Polycythemia also speaks of the disease. This is the name of a malignant tumor characterized by the proliferation of all cellular elements of the bone marrow.


An increased content of erythropoietin makes the blood thicker, clogs small vessels, and leads to disruption of the blood supply to the brain and heart, which is extremely dangerous for the body’s functioning. Exceeding the norm may indicate the following diseases of the skeletal system:
- blood loss;
- various forms of anemia;
- pure red bone marrow aplasia – the bone marrow produces leukocytes and platelets within normal limits, red blood cells – below acceptable limits;
- the initial stage of myelodysplastic syndrome - the disease is characterized by dysplastic changes in the bone marrow, combined with a lack of one or more types of blood cells, which can develop into acute leukemia;
- leukemia
Another reason for increased levels of the hormone is kidney disease, which produces erythropoietin. First of all, the amount of the substance increases when the blood supply to the kidneys is impaired due to shock, urolithiasis, polycystic kidney disease, or narrowing of the renal artery.
Some diseases that provoke an increase in erythropoietin cause a decrease in blood oxygen saturation. These are heart defects, congestive heart failure, and various lung diseases. Among them are chronic bronchitis, pneumoconiosis (incurable lung diseases caused by prolonged inhalation of industrial dust), chronic obstructive pulmonary disease, characterized by limited air flow in the respiratory tract.
An increase in erythropoietin in the blood can also signal the presence of a benign or malignant formation. This may be a malignant tumor of the central nervous system known as hemangioblastoma. The concentration of the hormone also increases in kidney tumors and pheochromocytoma (a tumor in the part of the adrenal cortex that is responsible for the synthesis of the hormones adrenaline and norepinephrine).
Doping in sports
Another reason why an increased amount of the hormone can be detected is the use of artificial erythropoietin in sports as a doping. Since the number of red blood cells increases under the influence of the hormone, blood begins to flow more intensively to all cells of the body, saturating them with nutrients and also charging them with energy.
A drug with a hormone analogue is especially popular in sports that require aerobic endurance - the ability of a person to do work of moderate intensity for a long time while the entire muscular system is functioning and to quickly recover after completion of the activity.

In this type of activity, oxygen is necessary to convert carbohydrates into energy; during particularly prolonged exercise, the body uses proteins and fats for this. These sports include cycling, long- and middle-distance running, and cross-country skiing.
But there is also a negative side to the use of a hormone analogue: recombinant erythropoietin in increased quantities depletes the body, disrupts its functioning and can lead to death. Therefore, after several deaths among cyclists, the drug was classified as a doping in 1990, after which erythropoietin was banned in sports.
Athletes who continued to use it after the ban were disqualified. This is exactly what happened in 2012 to the world famous cyclist Lance Armstrong: after discovering that he was taking doping and distributing it among athletes, the athlete was banned for life and stripped of all the awards he had won since 1998.
Determining the presence of alpha erythropoietin in the body is not easy, since it is very similar to the natural hormone. The drug, obtained by genetic engineering, is identical to natural erythropoietin in amino acid composition, but has differences in the structure of glucose elements.
Therefore, anti-doping laboratories use different methods for detecting doping in the blood. For example, in cycling, a restriction was introduced on the permissible level of hemoglobin, which is responsible for the transfer of oxygen to cells.


If during doping control the amount of hemoglobin in the blood exceeds the norm, the cyclist is removed from the competition. It cannot be denied that this is a very subjective indicator, largely dependent on the individual characteristics of the body, and hemoglobin above the norm does not always indicate the use of a forbidden drug.
Effective treatment
Erythropoietin analogue is produced by many pharmaceutical companies in five types: alpha, beta, omega, retard, theta. Alpha and beta are earlier drugs; theta hormone is considered the most effective: it is the least allergenic and has better purification. Erythropoietin omega differs more from other analogues from the human hormone, so it is easier to detect than others when testing for doping.
Drugs that contain erythropoietin are produced by different companies, so their effect is quite different from each other. Because of this, when switching from one drug to another, you need to study the instructions for use. If you use recombinant erythropoietin according to the instructions and prescriptions of your doctor, you can achieve good results in the treatment of many ailments, including: 
- chronic renal failure;
- malignant tumors;
- AIDS;
- tissue and organ transplantation;
- autodonation is the process of donating and preserving a patient’s blood before a planned operation, during which blood loss is possible;
- pre- and postpartum period without autodonation;
- various forms of anemia;
- in case of refusal of donor blood transfusion.
When using erythropoietin preparations, it is necessary to take into account that even the slightest fraction of the hormone has a huge impact on the body, since it affects changes in the rate of synthesis of this substance. Before using erythropoietin alpha, beta and other drugs, you must not only carefully follow the doctor’s instructions, but also carefully study the instructions for use.
The instructions provide for subcutaneous and intravenous administration of alpha erythropoietin. The goal of using the medicine is to achieve a level of blood cell volume in the blood from 30 to 35% and hemoglobin from 110 to 120 g/l (not higher). Blood should be donated for control during alpha erythropoietin therapy once a week.
If there is a need to increase the dose, the instructions allow this to be done no more than once every six months; each illness has its own maximum dose per week, which is not recommended to be exceeded. At the final stage of treatment, the dose is gradually reduced. When using the dosage of alpha erythropoietin indicated in the instructions, it must be taken into account that the use of other drugs may require a dose rate.
If tests show that erythropoietin increased by more than 20 g/l within four weeks, the dose of erythropoietin alpha, according to the instructions, should be reduced. If the patient has high blood pressure, cardiovascular diseases, as well as ailments associated with impaired cerebral circulation due to damage to the cerebral vessels of the brain, erythropoietin analogue should be prescribed with caution.
When using alpha erythropoietin, you must be prepared for the fact that two months after the hemoglobin level is normal, the analysis may show a lack of iron, folic acid, and vitamin B12. This can be easily corrected with a vitamin-mineral complex.